The project which was piloted in Jinja, Kamuli and Kitgum districts in the east and north of Uganda worked with primary health care services to increase access to support and treatment of substance use disorders, such as alcohol use disorder as well as mental health and neurological disorders.
An independent evaluation of the pilot indicates:
- Better community awareness has enabled 91% of people to recognize symptoms of MNS disorder.
- Some 67% of people with mental health concerns have sought treatment.
- mhGAP trained health workers regularly used mhGAP.
- Service users reported increased mental well-being.
The key intervention used in mhGAP is interpersonal therapy. The intervention has been successful in reducing people’s alcohol use problems and symptoms of depression and anxiety leading to better mental health and well-being.
The project has effected policy change as well. For example the Jinja district increased its annual mental health budget allocation.
Alcohol harm in Uganda
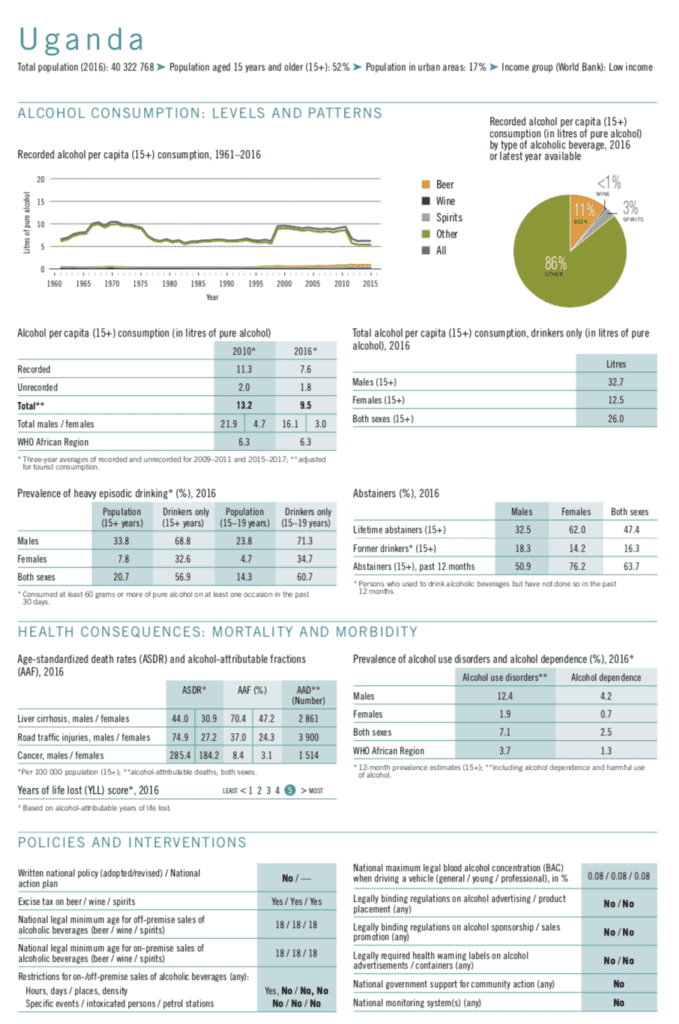
Uganda’s alcohol per capita consumption is higher than the WHO African region at 9.5 liters. Male alcohol users’ consumption is alarmingly high at 32.7 liters of pure alcohol per capita per year. Over half (56.9%) of all Ugandans above the age of 15 years who use alcohol engage in heavy episodic alcohol use.
The high male alcohol consumption has led to a heavy burden of alcohol harm.
- 12.4% Ugandan men suffer from an alcohol use disorder.
- 4.2% of Ugandan men are dependent on alcohol.
Uganda is placed on the highest end of the scale for years of life lost due to alcohol.
Despite the pervasive and heavy harm to Ugandans the country has for long not had a clear national alcohol policy system. This situation is likely to change as the Ugandan cabinet approved in September, 2019 the National Alcohol Control Policy (NACP). The making of NACP was a struggle fighting for public health amidst heavy Big Alcohol interference. Movendi International global voice David Kalema has detailed the journey towards the NACP in his blog post.
mhGAP for reduced alcohol harm and improved mental health
The above pilot projects have shown that integrating mental health services including substance use services into primary healthcare is low cost and effective. The interventions used were group interpersonal therapy, formation of active service user groups, stakeholder engagement, anti-stigma campaigns and advocacy for the protection of rights of service users.
These projects have scope for preventing and reducing alcohol harm and promoting mental health in Uganda. It also stands to show that such grassroot level interventions can change policies to support public health.
World Vision, with Uganda’s Ministry of Health and WHO, is now actively seeking support for wider scale up of the programme.
WHO Mental Health Gap Action Programme (mhGAP)
Mental, neurological, and substance use disorders are common in all regions of the world, affecting every community and age group across all income countries, according to the WHO.
While 14% of the global burden of disease is attributed to these disorders, most of the people affected – 75% in many low-income countries – do not have access to the treatment they need.
The WHO Mental Health Gap Action Programme (mhGAP) aims at scaling up services for mental, neurological and substance use disorders for countries especially with low- and middle-income. The programme asserts that with proper care, psychosocial assistance and medication, tens of millions could be treated for depression, schizophrenia, and epilepsy, prevented from suicide and begin to lead normal lives – even where resources are scarce.