The World Health Organization recently released its largest review of the world’s mental health. The review acts as a blueprint for governments, academics, health professionals, civil society, and others with an ambition to support the world in transforming mental health.
Key facts about the global mental health burden:
- In 2019, nearly a billion people – including 14% of the world’s adolescents – were living with a mental disorder.
- Suicide accounted for more than 1 in 100 deaths.
- 58% of suicides occurred before age 50.
- Mental disorders are the leading cause of disability, causing 1 in 6 years lived with disability.
- People with severe mental health conditions die on average 10 to 20 years earlier than the general population.
- Childhood sexual abuse and bullying victimization are major causes of depression.
- Structural threats to mental health include, social and economic inequalities, public health emergencies, war, and the climate crisis.
- Depression and anxiety increased by more than 25% in the first year of the COVID-19 pandemic alone.
Stigma and discrimination and human rights violations against people with mental health conditions are widespread problems. Even at present 20 countries consider attempted suicide a criminal offense. The poorest and most disadvantaged are at the highest risk of mental ill-health and are least likely to receive the care they need.
Mental health services are inadequate around the world. This is more pronounced in low and lower-middle-income countries.
- 71% of those with psychosis worldwide do not receive mental health services.
- 70% of people with psychosis are treated in high-income countries, and only 12% of people with psychosis receive mental health care in low-income countries.
- Even in high-income countries, only one-third of people with depression receive formal mental health care and minimally-adequate treatment for depression is estimated to range from 23% in high-income countries to 3% in low- and lower-middle-income countries.
Alcohol’s role in the global mental health burden
The new report cites older WHO estimates that 283 million people had alcohol use disorders in 2016 – a large mental health burden worldwide, given that overall 970 million people globally were living with a mental disorder in 2019.
The report addresses alcohol use as a risk factor that can undermine mental health, along with other risk factors such as genetics, low education, and an unhealthy diet.
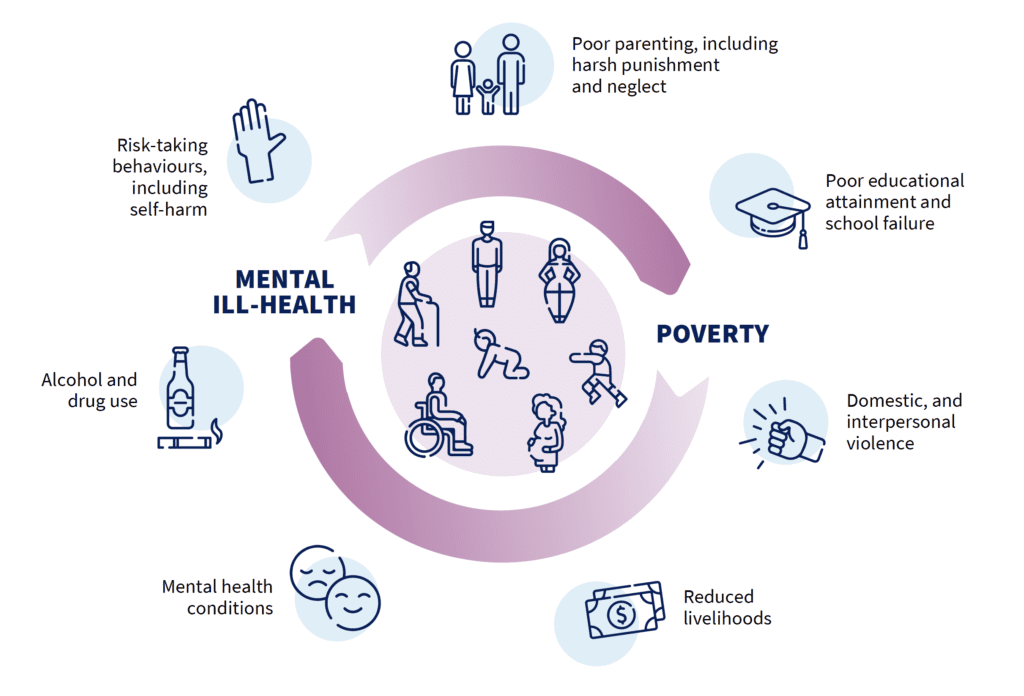
Alcohol use is highlighted as one of the risk factors which perpetuate the vicious cycle of mental ill-health and poverty.
The indirect costs related to mental health conditions can also be significant to countries. For example, in the Philippines, an analysis calculated that in 2019 six conditions (psychosis, bipolar disorder, depressive disorders, anxiety disorders, alcohol dependence and epilepsy) cost the national economy around US$ 1.3 billion in lost productive capacity due to premature death, disability and reduced productivity while at work.
The report includes alcohol use disorders as a mental health problem and treating AUD as part of the solution. Examples of investing in mental healthcare packages including for alcohol use disorders are included in the report.
For example, in South Asia and sub-Saharan Africa, the cost of scaling up delivery of an integrated package for epilepsy, depression, bipolar disorder, schizophrenia, and heavy alcohol use has been calculated at US$3 – $4 per capita. The return on investment for that would be 500 – 1000 healthy years of life for every million dollars spent.
Case studies from South Africa and Uzbekistan show investing in a mental healthcare package which included alcohol use disorders led to significant return on investment.
Furthermore, the report includes information about the WHO’s mhGAP intervention. Alcohol use disorders are one of the conditions targeted by the mhGAP. In Nepal’s Chitwan district mhGAP was implemented as part of a comprehensive mental health care plan. WHO mhGAP was able to increase treatment of mental health conditions including alcohol use disorders.
There is also information about the Alcohol e-Health self-help tool developed by the WHO. The tool is for people who want to reduce their alcohol use and it has so far been tested in Belarus, Brazil, India and Mexico with positive results in 6 months.
Reducing alcohol use is discussed under promoting healthy behaviors in order to build individual capital for mental health. Increasing public awareness about alcohol use and its effects and including alcohol addiction as part of an integrated package for mental health in the workplace are included strategies governments can use to promote healthy behaviors.
WHO recommendations to transform global mental health
This review by the WHO includes the latest evidence, examples of good practice, and voices people’s lived experiences. The report highlights where change is most needed and how it can be achieved.
The WHO calls on all stakeholders to work together to deepen the value and commitment given to mental health, reshape the environments that influence mental health, and strengthen the systems that care for people’s mental health.
The report calls for member states to accelerate their implementation of the Comprehensive mental health action plan 2013–2030 which was signed by all 194 member states. Even now, 2 out of every 3 dollars of scarce government spending on mental health is allocated to stand-alone psychiatric hospitals rather than community-based mental health services where people are best served. Mental health has so far not received enough attention, or resources from governments.
The report makes several recommendations grouped into the following three pathways of transformation:
- Deepen the value and commitment we give to mental health.
- Reshape environments that influence mental health, including homes, communities, schools, workplaces, health care services, and natural environments.
- Strengthen mental health care by changing where, how, and by whom mental health care is delivered and received.
Everyone’s life touches someone with a mental health condition. Good mental health translates to good physical health and this new report makes a compelling case for change,” said Dr. Tedros Adhanom Ghebreyesus, WHO Director-General, as per WHO News.
The inextricable links between mental health and public health, human rights, and socioeconomic development mean that transforming policy and practice in mental health can deliver real, substantive benefits for individuals, communities, and countries everywhere. Investment into mental health is an investment into a better life and future for all.”
Dr. Tedros Adhanom Ghebreyesus, WHO Director-General