Health-Care Spending Attributable to Modifiable Risk Factors in the USA: An Economic Attribution Analysis
Research article
Abstract
Background
There is a robust understanding of how specific behavioral (such as alcohol use), metabolic, and environmental risk factors increase the risk of health burden. However, there is less understanding of how these risks individually and jointly affect health-care spending.
The objective of this study was to quantify health-care spending attributable to modifiable risk factors, including alcohol, in the United States for 2016.
Methods
The researchers extracted estimates of US health-care spending by condition, age, and sex from the Institute for Health Metrics and Evaluation’s Disease Expenditure Study 2016 and merged these estimates with population attributable fraction estimates for 84 modifiable risk factors from the Global Burden of Diseases, Injuries, and Risk Factors Study 2017 to produce estimates of spending by condition attributable to these risk factors.
Because not all spending can be linked to health burden, the study adjusted attributable spending estimates downwards, proportional to the association between health burden and health-care spending across time and age for each aggregate health condition. The researchers propagated underlying uncertainty from the original data sources by randomly pairing the draws from the two studies and completing their analysis 1000 times independently.
Findings
In 2016, US health-care spending attributable to modifiable risk factors was US$ 730. 4 billion, corresponding to 27% of total health-care spending.
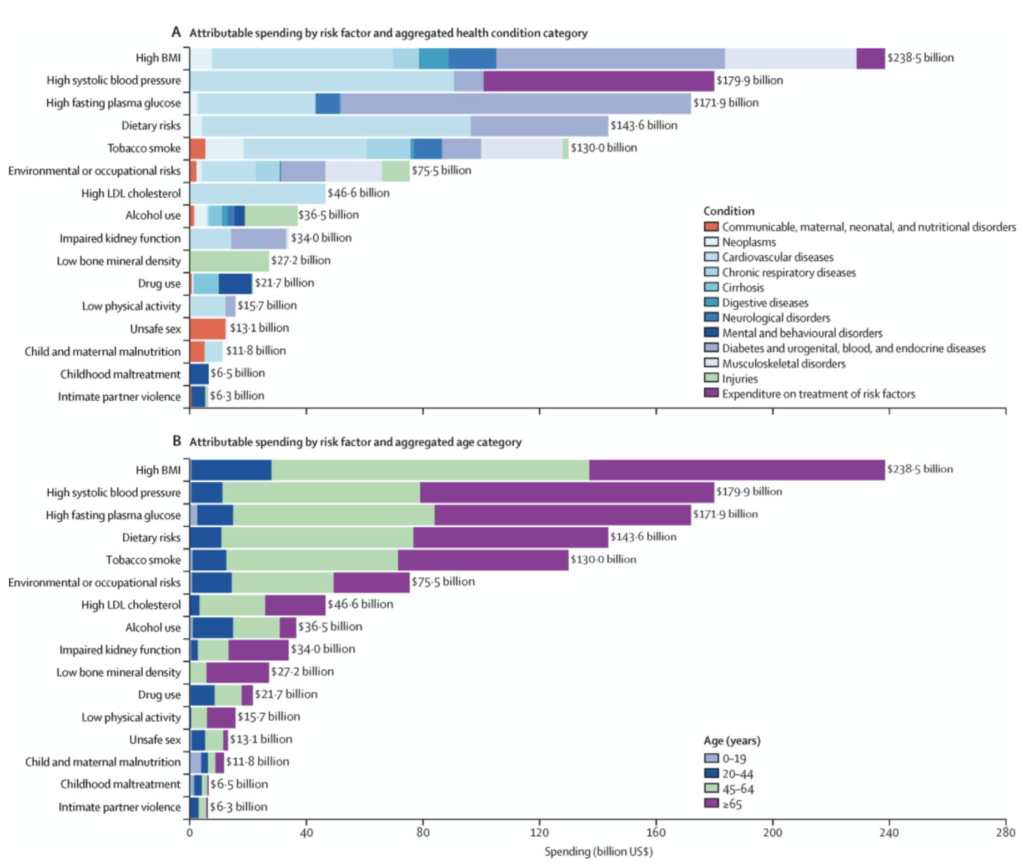
Attributable spending was largely due to five risk factors:
- high body-mass index ($238.5 billion),
- high systolic blood pressure ($179.9 billion),
- high fasting plasma glucose ($171.9 billion),
- dietary risks ($143.6 billion), and
- tobacco smoke ($130.0 billion).
Spending attributable to risk factor varied by age and sex, with the fraction of attributable spending largest for those aged 65 years and older (45.5%, 44.2–46.8).
Interpretation
This study shows high spending on health care attributable to modifiable risk factors and highlights the need for preventing and controlling risk exposure. These attributable spending estimates can contribute to informed development and implementation of programs to reduce risk exposure, their health burden, and health-care cost.
What the study finds regarding alcohol costs
At an aggregated risk level (level 1), metabolic risks were associated with the greatest attributable spending, at $508·0 billion in 2016. Behavioural risks, including dietary risks, alcohol use and tobacco smoke, had the second-highest attributable spending, at $349·4 billion.
Health-care spending attributed to risk factors by aggregated health condition category, 2016
Mental and substance use disorders
- Total spending: $180.7
- Attributable spending: $28.9
- Percentage of total spending: 16.0%
Alcohol costs massive among younger working age adults
Risk factor attributions varied greatly across the four aggregated age groups. The majority of total attributable spending was at older ages, with 86·7% occurring in people aged 45 years and older. But alcohol causes substantial costs (more than tobacco) in the younger working age population.
Attributable spending for working age adults was considerable. For younger working-age adults (ages 20–44 years) the greatest spending was for high BMI ($27·4 billion) followed by alcohol use ($13·8 billion), high fasting plasma glucose ($12·2 billion), tobacco smoke ($11·6 billion), and occupational risks ($11·1 billion). This age group contributed 12·9% of all attributable spending, and had 16·8% of health-care spending attributable to risk factors.
Alcohol costs in the bigger picture
The researchers found that the proportion of total health burden attributed to the modifiable risk factors considered in this study was substantially higher than the proportion of health-care spending attributed to those same risk factors – 46·2% versus 27·0%.
This discrepancy is due to the fact that several of the health conditions that have the most attributable health burden actually have relatively little health-care spending. Examples with little total spending but a large fraction of the attributable health burden were lung cancer ($7 billion in total health-care spending), drug use disorders ($13 billion), and alcohol use disorders ($8 billion).
In 2016, we estimated that US$730·4 billion, or 27·0% of total US health-care spending (included in the Disease Expenditure Project), was attributable to the modifiable risk factors included in this study, such as alcohol use.
The figure shows that alcohol contributes costs across a (the) big(gest) number of health conditions: communicable, maternal, neonatal and nutritional disorders, neoplasms, cardiovascular disease, cirrhosis, digestive diseases, neurological disorders, mental health and behavioral disorders, and injuries.
And the figure shows that alcohol use has a massive effect on the younger population, causing major costs in the age groups 20 to 44 and 45 to 64 – which are the ages when people are economically productive, but alcohol harm is jeopardizing economic acitivty.
In total, alcohol use causes $36.5 billion every year in health-care spending – a sum that could largely be avoided through alcohol policy solutions.