The EASL-Lancet Commission: Protecting the next generation of Europeans against liver disease complications and premature mortality
Key messages
- Liver disease is now the second leading cause of years of working life lost in Europe, after only ischaemic heart disease.
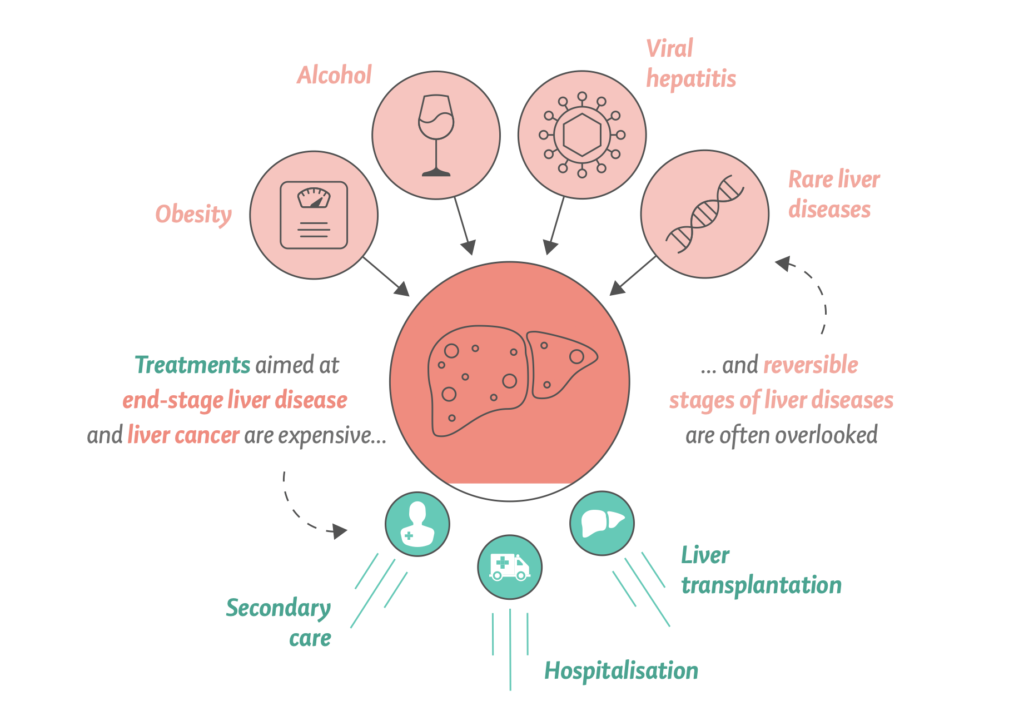
- The clinical focus in patients with liver disease is oriented towards cirrhosis and its complications, whereas early and reversible disease stages are frequently disregarded and overlooked.
- The dissociation between primary and secondary care and the considerable heterogeneity across clinical pathways and inconsistent models of care cause delays in diagnosis of both rare and common liver diseases.
- Stigma has a major impact on liver diseases in Europe, leading to discrimination, reduction in health-care seeking behaviour, and reduced allocation of resources, which all result in poor clinical outcomes.
- Europe has the highest level of alcohol consumption in the world, which, together with ultra-processed food consumption and high prevalence of obesity, are the major drivers of liver-related morbidity and mortality.
- A scarcity of consistent and efficient screening and vaccination programmes for viral hepatitis combined with the high costs of drugs due to variable European reimbursement systems result in reduced access to treatment and delays in elimination programmes.
- COVID-19, alongside imposing delays in diagnostic pathways of liver diseases, has brought overlapping metabolic risk factors and social inequities into the spotlight as crucial barriers to liver health for the next generation of Europeans.
- Liver diseases are generally avoidable or treatable if measures for prevention and early detection are properly implemented; achieving this would reduce premature morbidity and mortality, saving the lives of almost 300 000 people across Europe each year.
How the Liver Commission addresses alcohol
In Europe, alcohol consumption is by far the leading cause of liver-related mortality. Alcohol-related liver disease is the most frequent type of liver disease, being responsible for at least 50% of cirrhosis cases.
Europe has the highest level of alcohol consumption in the world, which, together with ultra-processed food consumption and high prevalence of obesity, are the major drivers of liver-related morbidity and mortality. More than 50% of end-stage liver disease is due to heavy levels of alcohol consumption.
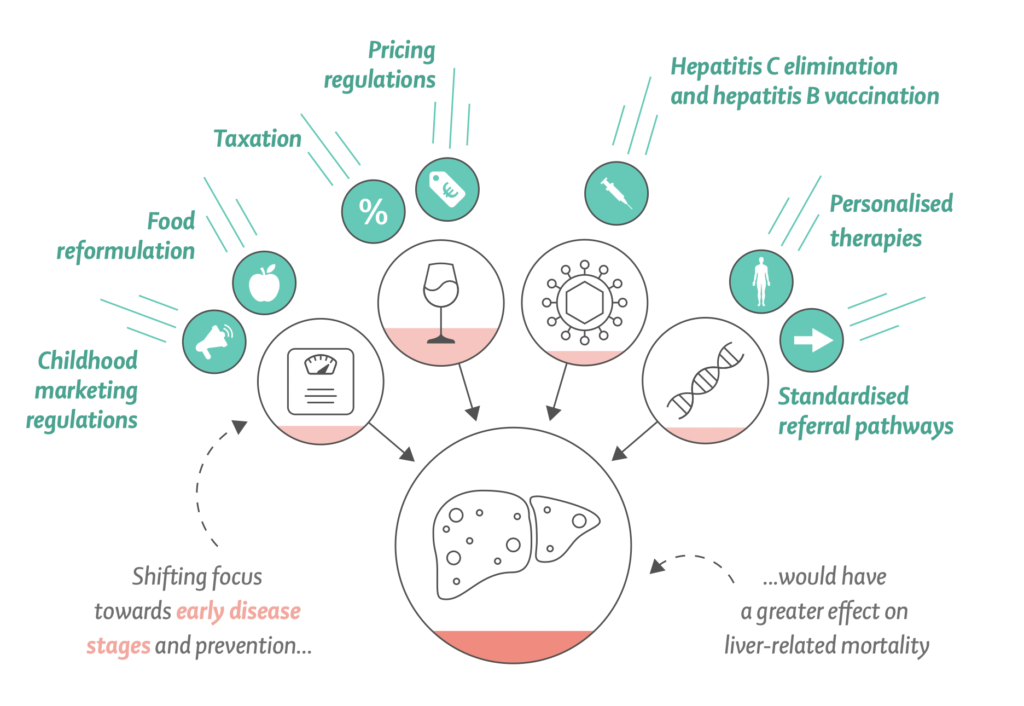
The Liver Commission says targeting end-stage liver disease with high-cost interventions is less effective at reducing liver-related mortality. Instead, the Liver Commission recommends a strategy focused on tackling the main causes of liver disease. Such an approach was cheaper to implement, and had a substantially greater effect.
The Liver Commission says targeting end-stage liver disease with high-cost interventions is less effective at reducing liver-related mortality. Instead, the Liver Commission recommends a strategy focused on tackling the main causes of liver disease. Such an approach was cheaper to implement, and had a substantially greater effect.
Mortality from alcohol-related liver disease is substantially greater for disadvantaged socioeconomic groups, particularly for younger patients, resulting in major health inequalities.
The COVID-19 pandemic has also brought with it physical restrictions that might create environments that lead to increased alcohol consumption. Recently, a U.S. study provided evidence for an alarming increase in Alcoholic Hepatitis associated with increasing heavy alcohol use during COVID-19 and highlighted the need for public health interventions around heavy alcohol consumption.
Such change in liver disease and deaths are entirely consistent with increases in alcohol consumption predominantly impacting on those with the highest alcohol intake. The case for action for liver disease is even stronger as a result.
Far beyond the liver, alcohol and ultra-processed foods represent key health challenges in the 21st century, and it is increasingly clear that liver disease acts as a cipher for health and a sentinel for our public health capacity.
Europe has the highest rates of alcohol consumption per person the highest prevalence of heavy episodic alcohol use, and the lowest rates of abstention from alcohol in the world. Alcohol combines synergistically with obesity and other risk factors for liver disease to drive the current high rates of end-stage liver disease and liver cancer. Alcohol causes about 40% of the 287,000 premature liver-related deaths in Europe every year, although the true number might be higher.
The OECD model projects:
- Healthy life expectancy to be ca. 1.3 years lower over the next 30 years because of deaths due to liver diseases, with 46% of the reduction as a result of alcohol consumption and 28% as a result of obesity.
- On average, 10.5 million life years and 8.8 million healthy life years will be lost every year in the EU27 + 5 because of liver disease.
- The average annual health expenditure for liver disease in the EU27 + 5 countries is €4.3 billion.
- The impact of liver disease on the economy of the same group of countries leads to the loss of the equivalent of 5 million full-time workers per year.
Alcohol policy solutions to prevent and reduce the liver disease burden in Europe
The Liver Commission argues that the liver is a window to the 21st-century health of the European population. Through the proposed syndemic approach to liver disease and social and health inequities in Europe, the liver will serve as a sentinel for improving the overall health of European populations.
The Liver Commission outlines how Europe can move forward with implementation of effective policy action on taxation, food reformulation, and product labelling, advertising, and availability, similar to that implemented for tobacco, to reduce consumption of alcohol, ultra-processed foods, and foods with added sugar, especially among young people.
COVID-19 has shown the need for public health action and the direct links that exist between population-level interventions, inequities, and mortality. Arguments often made to oppose such interventions have been refuted by the constant publishing of data showing their effectiveness in real time.
With regards to alcohol, the evidence for equitable public health policies is remarkably consistent, summarised by WHO as best buys:
- Tax increases on alcohol-containing beverages,
- Comprehensive restrictions and bans on alcohol marketing, and
- Restrictions on the availability of retailed alcohol.
Alcohol tax increases and minimum unit price for alcohol have implementation costs that are lower than the corresponding benefits in reduced health expenditure and increased labour force productivity. Alcohol taxes also generate revenues.
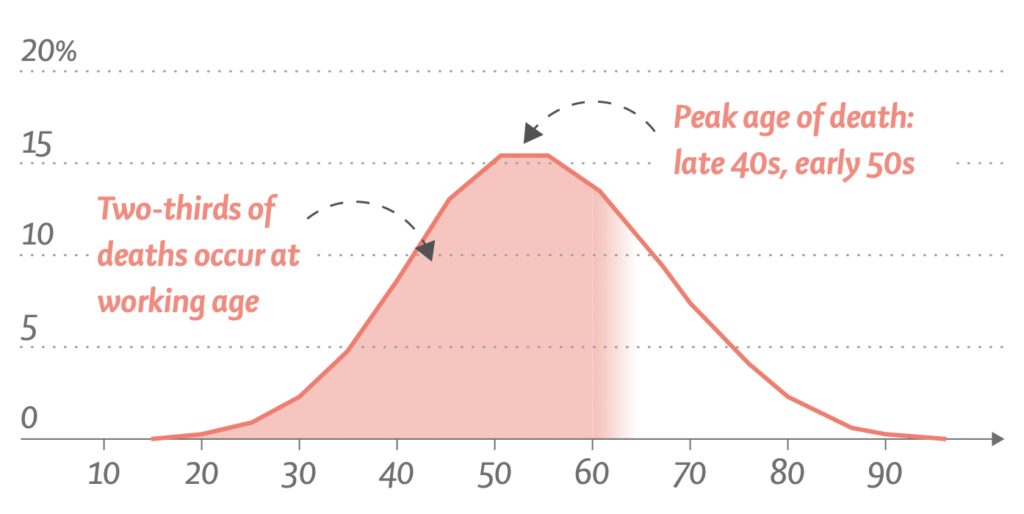
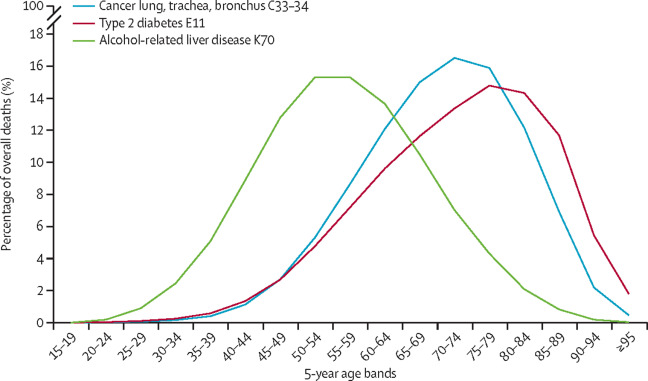
In Europe, chronic liver disease has a substantial impact on young and middle-aged individuals in their prime working years, with the peak age of death occurring in the late 40s and early 50s. This contrasts with mortality from smoking-related and other obesity-related illnesses, such as lung cancer or type 2 diabetes, for which deaths typically occur in the 60s and 70s.
Consequently, data from the World Health Organization shows that liver disease is now second only to ischemic heart disease as the leading cause of years of working life lost in Europe. On average, two-thirds of all potential years of life lost due to mortality from liver diseases are years of working life.
More details on how the Liver Commission addresses alcohol harm and policy solutions
- In Europe, alcohol consumption is by far the leading cause of liver-related mortality.
- Europe has the highest levels of alcohol consumption per person, the highest prevalence of heavy episodic alcohol use, and the lowest rates of abstention from alcohol in the world.
- Alcohol was responsible for around 580,000 deaths in 2019 (6.2% of all deaths) in the WHO European region, according to the Global Burden of Disease study modelling.
- Alcohol causes about 40% of the 287,000 premature liver-related deaths in Europe every year,
- but the true number is probably higher.
- Alcohol-related liver disease is the most frequent type of liver disease, being responsible for at least 50% of cirrhosis cases, and is the most common indication for liver transplantation in Europe.
- Nevertheless, research on alcohol-related liver disease is underrepresented, amounting to just 5% of all publications in the area of liver disease (2010–14 assessment).
- At the large European and American liver congresses, alcohol-related liver disease represented only 7% and 4%, respectively, of the research presented.
- Alcohol-related harm correlates with the volume and pattern of alcohol use, with epidemiological studies showing an exponential dose–response relationship between alcohol and liver disease.
- For most countries in the WHO European region, there is a strong correlation between liver-related mortality rates and population-level alcohol consumption.
- The evidence linking liver-related mortality and population-level alcohol consumption sends a crucial message for disease prevention:
- alcohol-related cirrhosis is a dose-related condition at the population level, and the most effectual and cost-effective means to reduce mortality rates from alcohol-related liver disease are interventions that reduce population-level alcohol consumption.
Executive Summary
Liver diseases have become a major health threat across Europe, and the face of European hepatology is changing due to the cure of viral hepatitis C and the control of chronic viral hepatitis B, the increasingly widespread unhealthy use of alcohol, the epidemic of obesity, and undiagnosed or untreated liver disease in migrant populations. Consequently, Europe is facing a looming syndemic, in which socioeconomic and health inequities combine to adversely affect liver disease prevalence, outcomes, and opportunities to receive care.
In addition, the COVID-19 pandemic has magnified pre-existing challenges to uniform implementation of policies and equity of access to care in Europe, arising from national borders and the cultural and historical heterogeneity of European societies. In following up on work from the Lancet Commission on liver disease in the UK and epidemiological studies led by the European Association for the Study of the Liver (EASL), this multidisciplinary Commission, comprising a wide range of public health, medical, and nursing specialty groups, along with patient representatives, set out to provide a snapshot of the European landscape on liver diseases and to propose a framework for the principal actions required to improve liver health in Europe.
The researchers believe that a joint European process of thinking, and construction of uniform policies and action, implementation, and evaluation can serve as a powerful mechanism to improve liver care in Europe and set the way for similar changes globally.
On the basis of these data, the researchers present ten actionable recommendations, half of which are oriented towards health-care providers and half of which focus primarily on health policy.
- Implementation of standardised and simplified liver blood tests for earlier detection and prompt care.
- Utilization of opportunities created by the hepatitis B and C drugs as well as hepatitis B and A vaccines to achieve viral hepatitis elimination in Europe.
- Increase awareness and provide financial incentives for primary care peers and professionals.
- Non-viral liver diseases must be classified along with other non-communicable diseases (NCDs) to engage appropriate care models.
- All forms and sources of stigma towards people at risk of or with liver disease must be opposed – relevant changes to the medical nomenclature should come first.
- Public disclosure of prices for antiviral drugs throughout Europe would reinforce the WHO / World Health Assembly resolution to improve fairness of market prices.
- European governments must introduce uniform policies to reduce harm due to alcohol.
- A complete social and digital media ban on the marketing of alcohol and ultra-processed, high-fat and high-sugar foods targeted to children.
- Promote industry-led food reformulation and minimisation of social inequities by subsidising healthy foods.
- EU and European governments should prioritise the harmonisation of critical forms of public health interventions and health-related policies across Europe.
A fundamental shift must occur, in which health promotion, prevention, proactive case-finding, early identification of progressive liver fibrosis, and early treatment of liver diseases replace the current emphasis on the management of end-stage liver disease complications.
A considerable focus should be put on underserved and marginalised communities, including early diagnosis and management in children, and we provide proposals on how to better target disadvantaged communities through health promotion, prevention, and care using multilevel interventions acting on current barriers.
Underlying this transformative shift is the need to enhance awareness of the preventable and treatable nature of many liver diseases. Therapeutic nihilism, which is prevalent in current clinical practice across a range of medical specialities as well as in many patients themselves, has to end. The researchers wish to challenge medical specialty protectionism and invite a broad range of stakeholders, including primary care physicians, nurses, patients, peers, and members of relevant communities, along with medical specialists trained in obesity, diabetes, liver disease, oncology, cardiovascular disease, public health, addictions, infectious diseases, and more, to engage in integrated person-centred liver patient care across classical medical specialty boundaries. This shift includes a revision in how we converse about liver disease and speak with our patients, and a reappraisal of disease-related medical nomenclature conducted to increase awareness and reduce the social stigmatisation associated with liver disease.
Reimbursement mechanisms and insurance systems must be harmonised to account for patient-centric, multimorbidity models of care across a range of medical specialties, and the World Health Assembly resolution to improve the transparency and fairness of market prices for medicines throughout Europe should be reinforced.
Finally, the researchers outline how Europe can move forward with implementation of effective policy action on taxation, food reformulation, and product labelling, advertising, and availability, similar to that implemented for tobacco, to reduce consumption of alcohol, ultra-processed foods, and foods with added sugar, especially among young people. It is important to utilise the window of opportunity created by the COVID-19 pandemic to overcome fragmentation and the variability of health prevention policies and research across Europe.
The researchers argue that the liver is a window to the 21st-century health of the European population. Through the proposed syndemic approach to liver disease and social and health inequities in Europe, the liver will serve as a sentinel for improving the overall health of European populations.