Alcohol and Blood Pressure
A REVIEW OF INTERNATIONAL AND SWEDISH RESEARCH
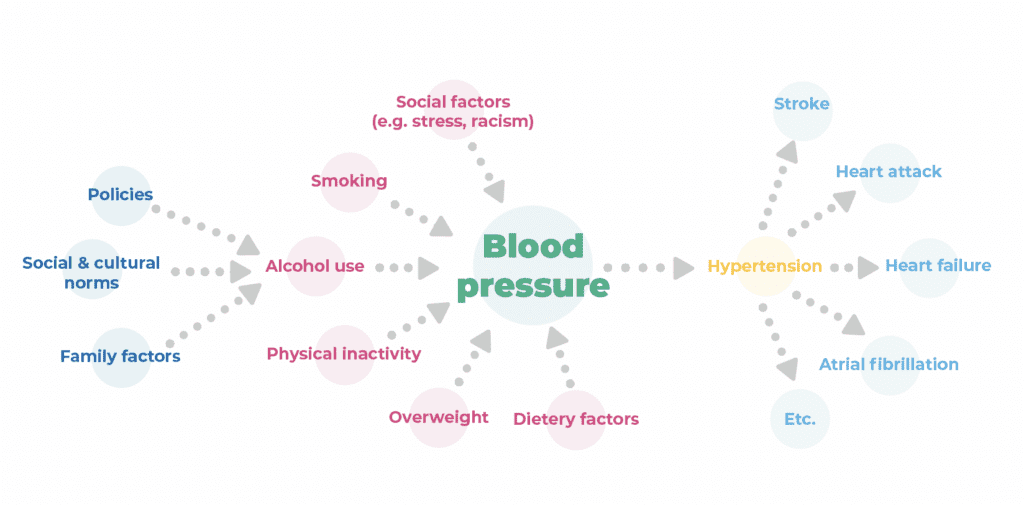
Alcohol is a significant contributing cause of hypertension. Hypertension itself is the leading cause of heart disease, stroke, type 2 diabetes and dementia.
How alcohol affects blood pressure negatively
Alcohol use affects the cardiovascular system negatively in multiple ways.
- The smooth functioning of the endothelium to maintain the capability to dilate the arteries in response to increased blood flow becomes gradually compromised with increased alcohol use, even for low-dose alcohol users and especially for people who consume alcohol heavily.
- Alcohol consumption causes calcification in both aortic and coronary arteries, increasing with level or dose of alcohol use.
- Chronic alcohol use impairs the important feedback system between the autonomic nervous system and the heart. This is an intricate regulatory system, consisting of nervous control of both vascular tone and heart rate.
- Binge alcohol use in adolescence, young adulthood and middle age predicts higher blood pressure at baseline and severalyears later.
The evidence is strong that alcohol use leads directly to elevated blood pressure in the short-term and hypertension in the longerterm without any safe level or protective effects.
- When people consume alcohol, mechanisms such as stiffness in arteries and increased wall thickness in blood vessels are strengthened, which lead to high blood pressure.
- High blood pressure increases the risk of a number of serious diseases and conditions such as heart attack, stroke, heart failure and kidney failure.
- Hypertension is a disorder of the circulatory system. It is the single largest threat to health and longevity globally.
- Hypertension is responsible for 10.8 million or 19.2% of deaths worldwide in 2019, largely due to various forms of cardiovascular disease.
The report synthesises the best research available. More and more studies with stronger methodology show only negative effects of alcohol consumption.
Alcohol increases the risk of ischemic heart disease, ischaemic and haemorrhagic stroke, atrial fibrilation, and cardiomyopathy.
- For example, estimates show that for every additional 10 grams of alcohol consumed per day, risk of atrial fibrillation increases by 8%.
- Combining mortality data across 103 countries, researchers estimated that alcohol caused about 5.6% of cardiomyopathy deaths.
- However, in countries where heavy alcohol use is highly prevalent, alcohol may be an underlying cause for more than 60% of all cardiomyopathy deaths.
Odds Ratio of alcohol and 6 cardiovascular disease phenotypes
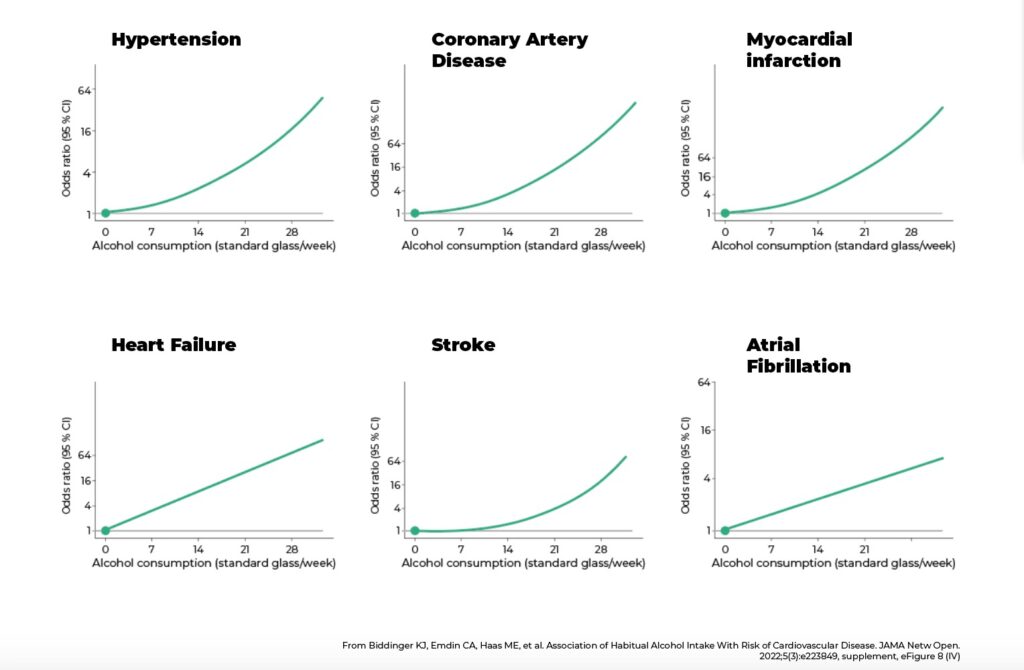
In the past, it was believed that low-dose alcohol use could protect against cardiovascular disease.
The new report is clear: There is no safe or reduced risk level of alcohol use concerning risk of hypertension in the longer term and this risk begins to escalate with increased consumption from even a low or moderate level.
The role of alcohol as a contributing cause of high blood pressure and cardiovascular disease is not well known by the public, by health care professionals or by decision makers. The report also shows that alcohol is seen by healthcare personnel as less important than physical activity, eating habits and smoking in preventing high blood pressure and other diseases.
High blood pressure is the single biggest preventable risk factor for disease and death in the world today, and alcohol’s contribution to high blood pressure is one of many overlooked factors,” says Frida Dangardt, senior physician and researcher at the Children’s Heart Center at Drottning Silvia’s Children’s Hospital in Gothenburg, who is one of the authors of the report.
If we can increase awareness of this connection among both the general public and within the health care system, much will be gained.”
Frida Dangardt, senior physician and researcher at the Children’s Heart Center at Drottning Silvia’s Children’s Hospital in Gothenburg
The researchers conclude that the most cost-effective way to reduce the incidence of high blood pressure, and the diseases that high blood pressure causes, is to introduce measures that reduce alcohol consumption in the population. Alcohol policy measures, such as higher alcohol tax and reduced availability of alcohol, are effective ways to keep alcohol consumption down and thereby reduce the risk of high blood pressure.
Why we know what we know
- Overall, alcohol consumption is a risk factor for high blood pressure. The connection is supported by studies of all types of methods and is most evident for consumption of more than 24 grams of alcohol per day.
- Results from cohort studies and studies with Mendelian randomization suggest that the risk of high blood pressure may increase even with very low consumption.
- There is no evidence that alcohol consumption at any level lowers blood pressure, or protects against high blood pressure, in randomized or cross-over studies.
Key messages
- Hypertension is a disorder of the circulatory system that represents the single largest threat to health and longevity globally.
- Alcohol is a significant contributing cause of hypertension. Hypertension itself is the leading cause of heart disease, stroke, type 2 diabetes and dementia.
- Alcohol’s role as contributing cause of hypertension has been neglected for too long.
- A recent policy brief from the World Heart Federation concluded that alcohol has played a major role in the near-doubling of theglobal prevalence of cardiovascular disease.
- Recognition of alcohol’s substantial causal role in the genesis of hypertension and related disease is belatedly being included in clinical guidelines for the management of high blood pressure.
- Physicians’ knowledge of lifestyle changes linked with improved health has been shown to be highest for taking regular exercise and reducing body weight and lowest for quitting smoking and reducing alcohol use.
- Alcohol’s causal role in hypertension is supported by (i) physiological research
- considering effects on the heart and blood vessels (ii) epidemiological research describing associations over time between alcohol use, blood pressure and hypertension.
- High quality clinical and experimental studies show that alcohol intake increases blood pressure.
- High quality epidemiological studies show alcohol intake aggravates mechanisms that lead to hypertension, such as inelasticity and thickness of arteries.
- High quality studies with randomization find no evidence that low level alcohol use has beneficial effects on blood pressure orhypertension.
- A growing number scientific critiques questions the hypothesis that alcohol in low doses can be cardioprotective.
- The value of evidence-informed prevention approaches to reducing individual health and societal burdens from hypertension hasnot yet been fully realised. Hypertension is largely a preventable disease and many modifiable risk factors have been identified.
- The World Health Organisation for example recommends reducing salt intake, eating more fruit and vegetables, getting more regular exercise, avoiding tobacco, reducing alcohol intake, limiting saturated fats and eliminating trans fats.
- Almost half of all people with hypertension remain unaware of their health status. Therefore it is necessary to point attention towards modifiable and highly prevalent risk factors for hypertension.
- The most cost-effective means of reducing hypertension and related health harms in a population are policies which reduce overall population alcohol consumption.
- Important improvements in blood pressure readings can be expected after as little as one month of going free from alcohol use.
Recommendations
When discussing population level changes in risks for hypertension, it is important to realise that even small reductions in mean blood pressure levels can translate into substantial reductions in related morbidity and mortality.
Alcohol should always be included in general health screening alongside assessments of other lifestyle risk factors relating to exercise, diet and smoking for example.
Physicians and other healthcare providers need training in how best to advise their patients to achieve their health goals.
Physicians and other healthcare providers also need to be supported by specialist advice and readily accessible support services.
It is essential that awareness of the causal association between alcohol use, hypertension and related serious diseases is raised substantially across the population at large, among healthcare providers and among decision-makers responsible for policies that affect the affordability, availability and acceptability of alcohol consumption.
- Governments should introduce policies to reduce the affordability, availability and acceptability of alcohol to reduce consumption and improve health.
- Implement effective policies including those that:
- maintain or increase alcohol prices (e.g. increased taxes, minimum unit prices),
- limit the physical availability of alcohol (e.g. restricted trading hours, placing restrictions on home delivery of alcohol, establishing higher minimum alcohol use age laws), and
- limit the social appeal of alcohol products (e.g. alcohol advertising restrictions and counter-marketing campaigns, requiring mandatory health warning labels).
- Governments should raise awareness of the links between alcohol and high blood pressure among the general public and health care providers.
- There is increasing consensus that requiring compulsory health warnings on all alcohol containers is a necessary first step to promote lower risk alcohol use and generate public support for effective population level alcohol policies.
- Provide adequate funding and resources to detect and address unhealthy alcohol use.
Health care systems and providers are the backbone of treatment for hypertension. Nevertheless, patients with existing hypertension are often not asked about their alcohol consumption or informed about how alcohol use might relate to their hypertension.
- Risks posed by alcohol consumption to elevated blood pressure and hypertension should be highlighted in clinical guidelines, on alcohol warning labels and in primary care interventions.
Provide advice on alcohol consumption in hypertension-related practice guidelines.
- Provide adequate incentives, including adequate financial compensation, for counselling and treatment related to alcohol use and/or alcohol use disorders.
- Develop better capacity and evidence-based standards for screening, brief intervention and also treatment of high-riskalcohol use and alcohol use disorders within primary care networks.
Individuals should reduce their alcohol use to no more than one Swedish standard alcoholic drink per day on most days and avoid more than two alcoholic drinks on a single occasion.
- For all drinkers, to minimise alcohol’s impact on health (including hypertension) and other social problems, it is especially important to avoid having four or more alcoholic drinks for men or women during an alcohol consumption occasion.
- For alcohol users with hypertension, particularly when blood pressure is not well controlled with other lifestyle interventions or medications, consider further reductions in alcohol use including a trial of avoiding any use to see if this helps control blood pressure.
About the report
A international group of esteemed researchers comes together every year to dive deeply into a specific topic of alcohol research.
First, the scientists conduct extensive research to identify relevant published science on the selected topic, such as alcohol and blood pressure.
Then, the group reviews and summarizes the search results. They are subsequently published in a report.
This year the report deals with alcohol and blood pressure – a topic of specific public interest due to the high health and mortality burden of hypertension and cardiovascular diseases, and due to pervasive misconcpetions and myths about alcohol’s role in heart disease.
The research group
- Sven Andreasson, senior physician and senior professor of social medicine at the department of global public health, Karolinska Institutet,
- Frida Dangardt, senior physician and researcher at the Children’s Heart Center at Queen Silvia’s Children’s Hospital in Gothenburg,
- Tanya Chikritzhs, PhD in alcohol epidemiology and leader of the alcohol research group at Australia’s National Drug Research Institute, NDRI,
- Tim Stockwell, researcher at, and former director of, the Canadian Institute for Substance Use Research in British Columbia, Canada,
- Timothy Naimi, physician and director of the Canadian Institute for Substance Use Research in British Columbia, Canada, and
- Harold Holder, Senior Scientist Emeritus and former Director of the Prevention Research Center (PRC), California.
The report disseminating partners
Dissemination of the report are IOGT-NTO, Movendi International, Riksförbundet HjärtLung, Swedish Association for General Medicine, Swedish Nurses Association, CERA, Stiftelsen Ansvar för Framtiden, Actis, Alcohol & Society, Hela människan, SLAN, MA – Rusfri Trafikk, MHF Motorförarnas Helnykterhetsbund , Sweden’s Blue Cross Association, Sweden’s Free Church Council, Swedish Association for Addiction Medicine, and SIGHT.