The cost of premature death from cancer attributable to alcohol: Productivity losses in Europe in 2018
Research article
Highlights
- An estimated 23,300 cancer deaths in people aged < 65 years in Europe in 2018 were due to alcohol.
- Premature deaths from alcohol-attributable cancer cost €4.58 billion in productivity losses.
- Productivity losses equalled 0.027 % of the total Gross Domestic Product of the 31 countries in 2018.
- Public health officials must prioritise implementation of cost-effective policies to reduce alcohol consumption and prevent alcohol-attributable cancer deaths.
Abstract
Background
More than 1.9 million people die from cancer each year in Europe. Alcohol use is a major modifiable risk factor for cancer and poses an economic burden on society.
The researchers estimated the cost of productivity lost due to premature death (under 65 years of age) from alcohol-attributable cancer in the European Union (EU) plus Iceland, Norway, Switzerland, and the United Kingdom (UK) in 2018.
Methods
The researchers estimated cancer deaths attributable to alcohol using a Levin-based population attributable fractions method and cancer deaths in 2018 from the Global Cancer Observatory.
Lost productivity was estimated for all alcohol-attributable cancer deaths by sex, cancer site, and country.
Productivity losses were valued using the human capital approach.
Results
An estimated 23,300 cancer deaths among people aged younger than 65 years in the EU plus Iceland, Norway, Switzerland and the UK in 2018 were attributable to alcohol (18,200 males, 5100 females).
This equated to €4.58 billion in total productivity losses in the region and 0.027 % of the European Gross Domestic Product (GDP).
The average cost per alcohol-attributable cancer death was €196,000.
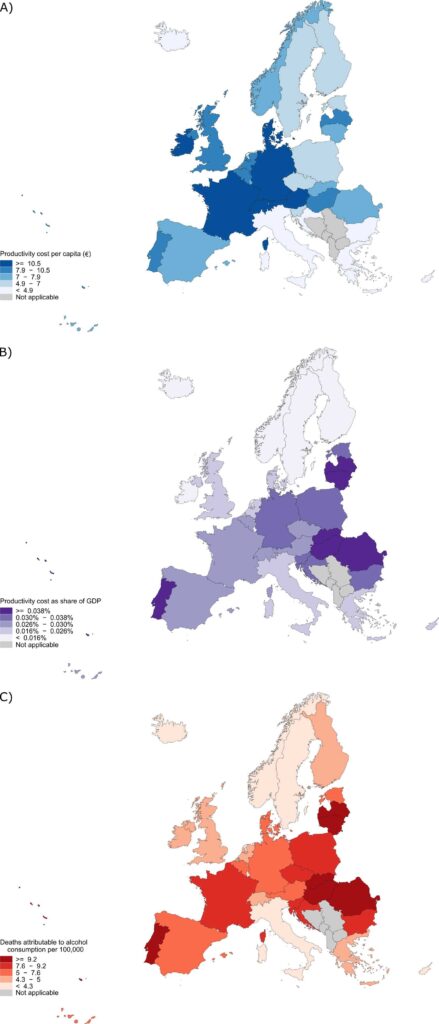
Productivity lost to alcohol-attributable cancer per capita was highest in Western Europe.
Hungary, Romania, Slovakia, Latvia, Lithuania, and Portugal had the highest rate of premature mortality from alcohol-attributable cancer and the highest productivity lost as a share of national GDP.
Conclusion
This study provides estimates of lost productivity from alcohol-attributable cancer death in Europe. Cost-effective strategies to prevent alcohol-attributable cancer deaths could result in economic benefits for society and must be prioritised.
Background
Cancer is a major burden of disease in Europe with nearly 4.4 million people diagnosed in the region every year. At least 1.9 million people die from cancer in Europe annually, and cancer deaths in the European Union (EU) are predicted to increase by 29 % by 2040, providing grounds for Europe’s Beating Cancer Plan.
Part of this plan encompasses reducing the use of alcohol which is higher in Europe than in other world regions. Alcohol is a causal factor for cancers of the oral cavity, pharynx, larynx, oesophagus, liver, colorectum, and breast.
Alcohol was responsible for an estimated 180,000 cases of cancer, or 4.5 % of all cases, in Europe in 2020.
As one of the most prominent modifiable risk factors for cancer, alcohol consumption has the potential to generate a high economic burden on society due to direct costs of health care or indirect costs such as loss of productivity from alcohol-attributable cancers.
Total productivity lost due to alcohol-attributable mortality from all alcohol-related diseases and injuries in the EU plus the United Kingdom (UK) has been estimated at €32.1 billion in 2016.
Quantifying the contribution of alcohol-attributable cancers to productivity losses would be of great value and provide a new perspective on the impact of risk factors on economic cost of disease.
Costs due to alcohol-attributable cancers have not yet been estimated.
Results
Premature cancer deaths attributable to alcohol in Europe
- In the 27 EU countries plus Iceland, Norway, Switzerland, and the UK, an estimated 23,300 cancer deaths among people aged less than 65 in 2018 were attributable to alcohol.
- Males represented 78 % of the total premature cancer deaths attributable to alcohol with approximately 18,200 cancer deaths.
- There were 5100 cancer deaths among females.
- The cancer sites which contributed the most alcohol-attributable deaths among males were:
- cancers of the colorectum (3400 deaths, 18.8 %),
- liver (3300 deaths, 17.9 %),
- pancreas (3200 deaths, 17.7 %) and
- oesophagus (3200 deaths, 17.3 %).
- The cancer sites which contributed the most alcohol-attributable deaths among females were:
- breast cancer (more than half of alcohol-attributable deaths, 2600 deaths, 50.7 %), followed by
- colorectal cancer (770 deaths, 15.1 %) and
- pancreatic cancer (510 deaths, 10.0 %).
Within Europe, countries in Western Europe contributed the largest number of premature cancer deaths attributable to alcohol with a total of 8800 cancer deaths (37.9 % of all deaths in the 27 EU countries plus Iceland, Norway, Switzerland, and the UK).
Relative to population size, Central and Eastern Europe had the highest burden of premature cancer mortality attributable to alcohol consumption (10.8 deaths per 100,000 people); this was also the case when comparing rates for males and females (17.3 and 4.2 deaths per 100,000 men and women, respectively, in Central and Eastern Europe).
Productivity losses due to premature cancer deaths attributable to alcohol in Europe
The total value of productivity losses due to premature cancer deaths attributable to alcohol in 2018 was €4.58 billion.
Premature cancer deaths among males contributed €3.69 billion in productivity losses (81 %) with the remaining €890 million from females (19 %).
The costliest cancer sites in terms of total productivity losses were cancers of the colorectum (€799 million), pancreas (€740 million), liver (€717 million), and oesophagus (€697 million).
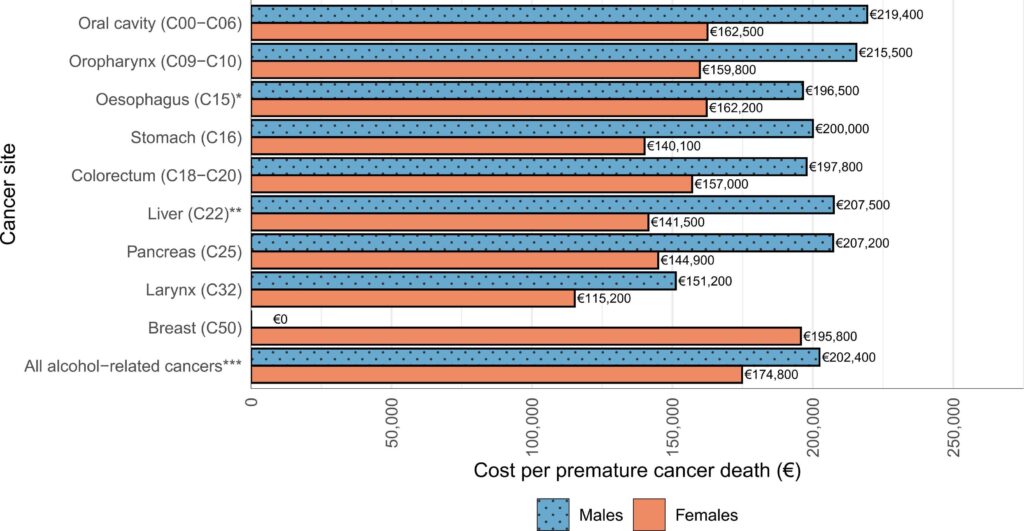
The average cost per alcohol-attributable premature cancer death was €196,000.
The costliest cancer sites among males were cancers of the oral cavity (€219,000/death) and oropharynx (€216,000/death).
Among females, the costliest cancer site per premature death was breast cancer (€196,000/death) followed by oral cavity cancer (€163,000/death) and oesophageal cancer (€162,000/death).
Regional and national productivity losses due to premature cancer deaths attributable to alcohol
The burden of alcohol-attributable cancer deaths and productivity lost differed between countries and regions within Europe.
The total productivity lost to premature mortality from alcohol-attributable cancer was largest in Western Europe at €2.37 billion.
76 % of the total productivity lost to premature mortality from cancers due to alcohol was represented by Germany (€1.12 billion) and France (€695 million).
The total cost of alcohol-attributable cancer mortality among the European regions was lower in Northern Europe (€877 million) and Southern Europe (€801 million), and Central and Eastern Europe (€529 million).
Relative to population size, total productivity cost per capita was highest in Switzerland (€18.90 per person), Germany (€13.60), and Austria (€13.00), resulting in Western Europe as the region with the highest productivity cost per capita (€12.20).
Conversely, countries in Southern and Central and Eastern Europe had the lowest cost per capita including Malta, Bulgaria, Cyprus, Greece, Croatia, and Italy which had productivity costs less than €5 per capita.
In all countries, the cost of productivity lost to premature death from alcohol-attributable cancer per capita was higher for males than females. The countries with the largest cost per premature death from alcohol-attributable cancer were Switzerland (€582,600/death), Norway (€418,000/death), Ireland (€374,000/death), and Denmark (€358,700/death).
The total cost of productivity lost to alcohol-attributable cancer as a share of the combined GDP of the EU plus Iceland, Norway, Switzerland, and the UK was 0.027 %.
The countries with the highest cost of productivity lost as a share of national GDP were Hungary, Romania, Slovakia, Latvia, Lithuania, and Portugal (all between 0.045 % and 0.069 % of GDP) which corresponded with the countries which had the highest rate of premature cancer death attributable to alcohol.
The countries with the lowest cost of productivity as a share of GDP were Malta (0.001 %), Luxembourg (0.008 %), and Norway and Sweden (both 0.011 %).
Conclusions and way forward
Europe has the highest levels of alcohol consumption per capita in the world which has led to a substantial burden of cancer attributable to alcohol.
Recent estimates show paid productivity losses due to premature mortality from cancer reached a total of €52.9 billion in the EU plus Iceland, Norway, Switzerland, and the UK in 2018. The study’s main finding of €4.58 billion lost to alcohol-attributable cancer represents 9 % of this total.
The researchers found a higher average cost per death in the current study compared to the earlier study (€196,000 versus €152,000). As the same data sources and methodology were used to calculate productivity losses in both studies, the higher cost per death could be a result of younger age at death from alcohol-attributable cancers and the combination of a predominantly male burden of alcohol-attributable cancer deaths – largely due to men in Europe consuming around three times the volume of alcohol per person as women – with higher rates of labour market participation and wages among men than women in Europe.
Our results are certainly an underestimate of the total loss of productivity due to alcohol-attributable cancer deaths. Ortega-Ortega et al. found that losses in unpaid employment due to premature cancer death contributed nearly 50% of the total losses in productivity, taking the total cost of productivity lost due to cancer up to €104.6 billion.
The researchers did not estimate unpaid productivity costs because they did not have access to estimates of unpaid production and time spent on unpaid tasks, but they would expect the total cost of productivity lost to markedly increase if including unpaid employment. Other productivity losses which could be considered in future analyses — if appropriate data become available — are losses due to impaired working and absenteeism of an employee, such as temporary work absences or reduced working capacity due to cancer symptoms or treatment, as well as wider productivity loss among cancer caregivers e.g. close family members while they accompany cancer patients during their treatments or provide care at other times. Other productivity loss analyses could include use of the friction cost approach which assumes the economy replaces those who die or are unable to work due to illness, thus the productivity lost by the employer only occurs at the time when the work isn’t done or while replacing the worker.
For overall alcohol-related costs, a systematic review of mainly European and North American studies found a third of the economic costs of alcohol use to society were direct, including the cost of health care, the criminal justice system, and road traffic accidents, but productivity losses including premature mortality and impaired productivity in the workplace were the main driver of cost (61.2 % of estimated cost). Future studies on the cost of alcohol-attributable cancers which incorporate both direct and indirect costs would be of value to estimate their full economic and societal impact.
Alcohol policy for cancer prevention
This economic assessment complements — and provides an important backdrop for — cost-effectiveness analyses conducted to set priorities in alcohol control, such as policies proposed by the WHO as part of their ‘best buys’ for tackling non-communicable diseases.
The most cost-effective policies were determined through weighing up dollars spent on policy implementation versus gain in healthy life year; the policies deemed most cost-effective were an increase in excise taxes and the enactment and enforcement of restrictions to purchasing availability and marketing.
As part of Europe’s Beating Cancer Plan, the European Commission has committed to review EU legislation on alcohol taxation and alcohol marketing to young people. Other WHO-recommended alcohol policy strategies include minimum unit pricing, adding cancer warning labels to alcohol products, and giving brief advice to patients in primary care. The EU Commission also indicated that it will review its policy on pricing of alcoholic beverages and propose mandatory health warnings on labels on alcoholic beverages before the end 2023, and provide support for Member States to implement evidence-based brief interventions on alcohol in primary care as well as the workplace and through social services.
Additionally, measuring the impact of changes in alcohol policy on cancer burden would provide further evidence for prioritisation of cancer prevention strategies. The impact of increases in alcohol excise taxes on cancer burden in Europe has already been modelled, but these assessments have not yet been supplemented with the costs of alcohol-attributable cancers which could expand future cost-effectiveness analyses of alcohol control or cancer prevention policies.
This study provides further economic reasoning to curb the burden of alcohol-attributable cancer and drive action to achieve the reduction in alcohol use set out in Europe’s Beating Cancer Plan.
This analysis adds a new perspective to assessments of alcohol-attributable cancer burden, and complements policy impact assessments such as those carried out on the potential reduction in cancer burden following increases in alcohol excise taxes.
The implementation of cost-effective policies to reduce alcohol consumption and prevent alcohol-attributable cancer deaths could result in economic benefits for society and must be prioritised.
