Alcohol rehabilitation and cancer risk: a nationwide hospital cohort study in France
Research article
Background
Alcohol consumption is linked to multiple diseases and injuries, including several cancer sites:
- oral,
- pharyngeal,
- laryngeal,
- oesophageal,
- liver (hepatocellular),
- colorectal, and
- female breast cancers.
The burden of cancer due to alcohol is substantial and accounted for 4.1% of all new cases of cancer globally in 2020.
Men accounted for approximately three-quarters of alcohol-attributable cancer cases due to their higher average alcohol consumption.
A reduction or cessation of alcohol consumption should result in a reduction in the burden of cancer due to alcohol.
Evidence before this study
In 2023, the International Agency for Research on Cancer (IARC) convened an International Expert Working Group to review published studies and evaluate the strength of epidemiological and mechanistic evidence on the potential for alcohol reduction or cessation to reduce alcohol-attributable cancer risk. They found “sufficient evidence” for only two cancer sites (oral and oesophageal cancers), and “limited evidence” or “inadequate evidence” for other alcohol-attributable cancer sites.
Overall, few studies exist on this topic, and even fewer high-quality studies with sufficient statistical power and adequate control for tobacco smoking as the main confounder.
Added value of this study
There is little evidence available on the role of alcohol reduction or cessation in reducing cancer risks. Moreover, there are almost no studies – and therefore no evidence – on the role of rehabilitation and abstinence in reducing cancer risks for people with alcohol dependence and heavy alcohol use.
However, this evidence is crucial for policy makers to inform targeted interventions and policies aimed at cancer prevention.
Using a representative large cohort of all 25.3 million adults discharged from French hospitals between 2018 and 2021, the researchers found a strong association between alcohol dependence and the risk for each alcohol-associated cancer site in both sexes, except for breast cancer.
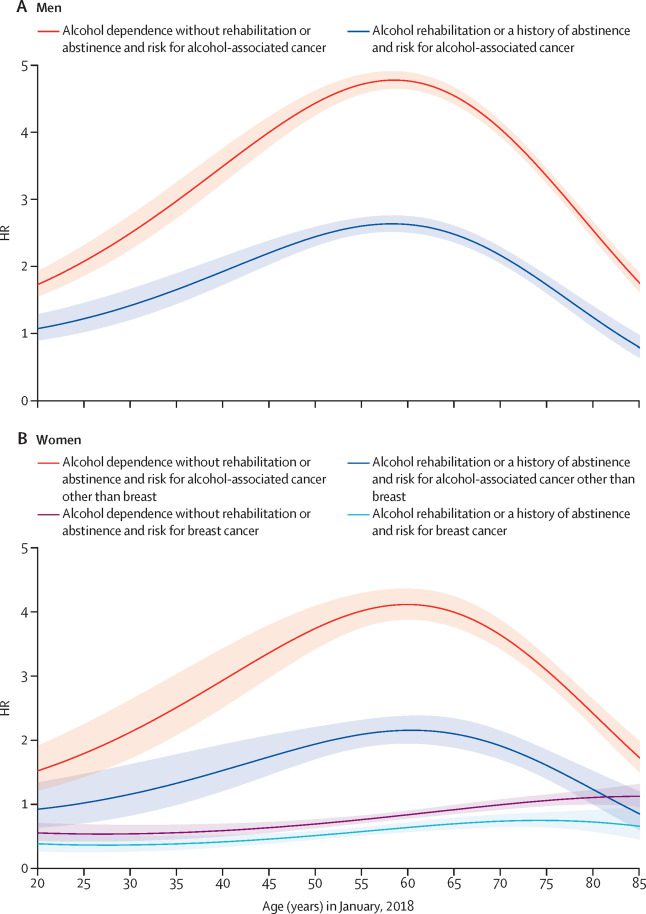
Rehabilitation treatment at hospital or a history of abstinence was linked to large benefits among patients with alcohol dependence, with about 40% relative reductions in the risk for cancers due to alcohol in both sexes.
Relative risk reductions were significant for each cancer site (hepatocellular carcinoma and oral, pharyngeal, laryngeal, oesophageal, colorectal, and breast cancer) and in all socioeconomic groups.
Relative reductions in the risk for cancer due to alcohol were even higher in patients having only a recorded history of abstinence compared with those receiving rehabilitation treatment at hospital, supporting that the benefits of alcohol reduction or cessation increase over time.
The strengths of this study
The French National Hospital Discharge database offers a unique opportunity to fill some of these research gaps, especially given that the average annual level of adult alcohol consumption per capita in France (11.0 L of pure alcohol) was over twice the global average (5.3 L) in 2018–20.
Accordingly, a large number of patients with alcohol dependence – ie, the most severe form of alcohol use disorders – are diagnosed and cared for in acute care or specialised hospitals in France. In addition, all patients diagnosed with cancer are treated at hospital.
Purpose of the study
The study aim was to test two main hypotheses for cancers due to alcohol, overall and by cancer site:
- alcohol dependence is associated with an increased risk compared with no alcohol dependence; and
- rehabilitation treatment or a history of abstinence is associated with a decreased risk compared with alcohol dependence without rehabilitation or abstinence.
Implications of all the available evidence
Alcohol rehabilitation, which is linked to at least temporary reduction or cessation of alcohol consumption, was linked with a substantially lower risk in incidence of cancer due to alcohol.
Unfortunately, this intervention was only given to a minority of patients in French hospitals. To prevent future cancers, alcohol rehabilitation should be offered and used more widely.
Detailed results
Of the 49,175,541 adults residing in mainland France on Jan 1, 2018, 25,291,344 (51.4%) were discharged from acute, post-acute, or psychiatric hospitals in 2018–21.
Alcohol dependence was identified in 645,720 (6.3%) of 10,260,056 men and 219,323 (1.6%) of 13,739 369 women.
Among patients with alcohol dependence, the proportions of patients with a record of rehabilitation treatment or a history of abstinence were similar across sexes (men: 245,550 [38.0%]; women: 87,723 [40.0%]).
Of them, 141,682 (57.7%) men and 48,167 (54.9%) women had used rehabilitation services at hospital with a median follow-up of 3.8 years since the first treatment in 2013–21, and other patients were only recorded with a history of abstinence in 2013–21. The median length of inpatient stay was 13 days for rehabilitation treatment.
Alcohol dependence categories were associated with higher area deprivation, previous hospital admission(s) in 2013–17, any cancer risk factor, and in-hospital death in 2018–21 in both sexes.
Patients identified with rehabilitation treatment or a history of abstinence had the highest rates of cancer risk factors, including tobacco smoking and chronic hepatitis C infection, in both sexes.
Overall, 602,199 (2.5%) patients were newly diagnosed in 2018–21 with cancer sites identified as being causally related to alcohol consumption.
Cancers due to alcohol included heterogeneous cancer sites, with sites differing in frequency, sex ratio, median age at diagnosis, and prognosis.
Alcohol dependence was more frequently recorded in men than in women for all cancer due to alcohol sites and categories:
- hepatocellular carcinoma (men: 14,621 [51.3%]; women: 2036 [25.7%]),
- upper aerodigestive tract cancers (men: 16,743 [27.5%]; women: 3031 [15.0%]), and
- colorectal cancer (men: 7795 [7.5%]; women: 1958 [2.1%].
Alcohol dependence without any hospital record of rehabilitation treatment or abstinence in 2013–21 was a major risk factor for all cancer due to alcohol in both sexes, except for breast cancer.
Rehabilitation treatment or a history of abstinence was associated with lower risks compared with alcohol dependence without rehabilitation or abstinence, with about 40% relative reductions in the risk for cancer due to alcohol.
Relative risk reductions were significant for each cancer site or category in both sexes.
The benefits of alcohol rehabilitation and abstinence on cancer due to alcohol risk were supported by all subgroup and sensitivity analyses. Relative reductions in the risk for alcohol-associated cancer were similar in population subgroups defined by area deprivation index quintile or residency in a territory covered by a cancer registry.
Compared with 13,853,542 patients with previous hospital admission(s) in 2013–17, 10,145,883 patients newly discharged in 2018–21 were, as expected, younger (median age of 51 years vs 58 years on Jan 1, 2018) and less comorbid (alcohol dependence: 218,790 [2.2%] vs 646,253 [4.7%]; any cancer risk factor: 1,219,629 [12.0%] vs 3,543,461 [25.6%]).
Alcohol dependence without rehabilitation or abstinence was similarly associated with increased risks for alcohol-associated cancer in both population subgroups. In contrast, relative risk reductions with rehabilitation or abstinence were even higher in patients newly discharged in 2018–21 compared with those with previous hospital admission(s) in 2013–17.
Patients recorded with wholly alcohol-attributable disease were at increased risk for alcohol-associated cancer compared with other patients recorded with alcohol dependence, although the benefits of rehabilitation and abstinence on alcohol-associated cancer risk were similar in both patient groups.
The researchers also found that relative reductions in the risk for cancer due to alcohol were even higher in patients having only a recorded history of abstinence compared with those receiving rehabilitation treatment at hospital in 2013–21.
With the exception of breast cancer, the researchers found that rehabilitation treatment or a history of abstinence was associated with decreasing risks for cancer due to alcohol over the lifespan, with maximum benefits seen in middle-aged patients.
Conclusions and implications
In this nationwide hospital cohort study, the researchers found a marked link of alcohol dependence with cancers due alcohol after controlling for potential confounding risk factors.
The study results also support the benefits of alcohol rehabilitation and abstinence in reducing the risk for cancers due to alcohol, overall and for each cancer site.
The study results corroborate and expand on previous studies, which were limited to cancer risks associated with different levels of alcohol consumption recorded at cohort inception.
Alcohol dependence is strongly associated with heavy alcohol use (>60 g of pure ethanol per day, the equivalent of more than six alcoholic drinks per day) and thus – with the exception of female breast cancer – has predictably been linked in this study with risks at the high end of the exponential dose–response curve for cancers due to alcohol.
Alcohol rehabilitation or abstinence should be associated with a decreased risk for any alcohol-associated cancer but the evidence is scarce and limited, while a recent study on patterns of alcohol consumption over the life course suggested that heavy alcohol use remains associated with higher risks for cancers due alcohol, despite alcohol reduction or cessation.
The study results support that the benefits of alcohol reduction or cessation increase over time as the study found that relative reductions in the risk for cancer due to alcohol were even higher in patients having only a recorded history of abstinence compared with those receiving rehabilitation treatment at hospital in 2013–21.
Overall, the study results point to a potent effect of alcohol rehabilitation and abstinence to reduce cancer due to alcohol risks. While the hospital cohort study involved a large sample of the French adult population, the study results were robust across sexes and in all other subgroup or sensitivity analyses, supporting high generalisability to the whole population. Accordingly, future editions of the IARC Handbooks of Cancer Prevention might include more alcohol-associated cancer risks where there is sufficient evidence for a positive effect derived from reduction or cessation of alcohol consumption.
Only 333,273 (38.5%) of 865,043 patients with alcohol dependence and discharged from French hospitals in 2018–21 had received rehabilitation treatment at hospital or were recorded with a history of abstinence in 2013–21. In 2007, the French Government aimed to improve hospital-based addiction care by implementing financial incentives that are all captured in this study. However, for a variety of reasons including persisting stigma and a shrinking medical workforce, the provision of rehabilitation services at hospital often remains limited to the most severe or comorbid patients with alcohol dependence.
The researchers found indeed that rehabilitation treatment at hospital or a history of abstinence were disproportionately recorded in older and more comorbid patients with previous hospital admission(s) in 2013–17, although relative reductions in the risk for alcohol-associated cancer were much higher in patients newly discharged in 2018–21. Accordingly, the benefits of rehabilitation treatment should be expected to be larger if extended to an earlier stage of alcohol dependence.
The results of the study also suggest that observed reductions in alcohol-attributable cancer risk were similar across population subgroups defined by area deprivation index quintile, emphasising the importance of alcohol rehabilitation services for reducing health inequalities.
In conclusion, effective alcohol interventions are underused in French hospitals, as is the case elsewhere.
Screening for alcohol consumption at hospital, followed by brief interventions for hazardous alcohol intake or with rehabilitation treatment for alcohol use disorders is a major step towards preventing many cancer cases.
In addition, delivering routine screening and outpatient interventions upstream in primary health care should also be considered.
However, considering the relatively high costs of all individual-level interventions, cancer prevention should start with the implementation of population-level strategies, which aim to reduce alcohol consumption and alcohol-attributable burden of disease, including cancer, across the entire population. These are WHO’s so-called best buys – ie, raising taxes to make alcohol less affordable, reducing availability, and banning marketing.
Abstract
Background
Even though alcohol consumption is an established risk factor for cancer, evidence regarding the effect of a reduction or cessation of alcohol consumption on cancer incidence is scarce.
The main study aim was to assess the effect of alcohol rehabilitation and abstinence on cancer incidence in people with alcohol dependence.
Methods
The researchers conducted a nationwide hospital retrospective cohort study which included all adults residing in mainland France and discharged in 2018–21.
Multivariable Cox proportional hazards models were used to estimate the effect of rehabilitation treatment at hospital or a history of abstinence versus alcohol dependence without rehabilitation or abstinence on the risk for incident alcohol-associated cancers by sex, controlled for potential confounding risk factors.
Findings
10,260,056 men and 13,739,369 women were discharged from French hospitals in 2018–21. Alcohol dependence was identified in 645,720 (6.3%) men and 219,323 (1.6%) women.
Alcohol dependence was strongly related to alcohol-associated cancer sites in both sexes (hepatocellular carcinoma and oral, pharyngeal, laryngeal, oesophageal, and colorectal cancers), except for breast cancer.
Rehabilitation treatment or abstinence was associated with significantly lower risks compared with alcohol dependence without rehabilitation or abstinence.
Relative risk reductions were significant for each alcohol-associated cancer site in both sexes and supported by all subgroup and sensitivity analyses.
Interpretation
The study results support the clear benefits of alcohol rehabilitation and abstinence in reducing the risk for alcohol-associated cancers.
As only two in five patients with alcohol dependence were recorded with a history of rehabilitation treatment or abstinence, a large untapped potential exists for reducing cancer incidence.