The future health of Europeans is inextricably related to a fundamental shift in the way in which liver disease needs to be prevented, diagnosed and treated, an expert panel of health professionals from various medical disciplines, nurses and patients has concluded after a three-year analysis.
The EASL-Lancet Liver Commission: Protecting the next generation of Europeans against liver disease complications and premature mortality (The Commission), has released its report.
The Liver Commission recommends that Europe’s fragmented health policies and health systems need to become more integrated, coordinated and effective to enable earlier detection of disease and to bring common risk factors for liver disease, such as alcohol and obesity, under control.
In Europe, alcohol consumption is by far the leading cause of liver-related mortality. Alcohol-related liver disease is the most frequent type of liver disease, being responsible for at least 50% of cirrhosis cases.
Europe has the highest level of alcohol consumption in the world, which, together with ultra-processed food consumption and high prevalence of obesity, are the major drivers of liver-related morbidity and mortality. More than 50% of end-stage liver disease is due to heavy levels of alcohol consumption.
Addressing liver disease risk factors means creating healthy environments and reducing inequity
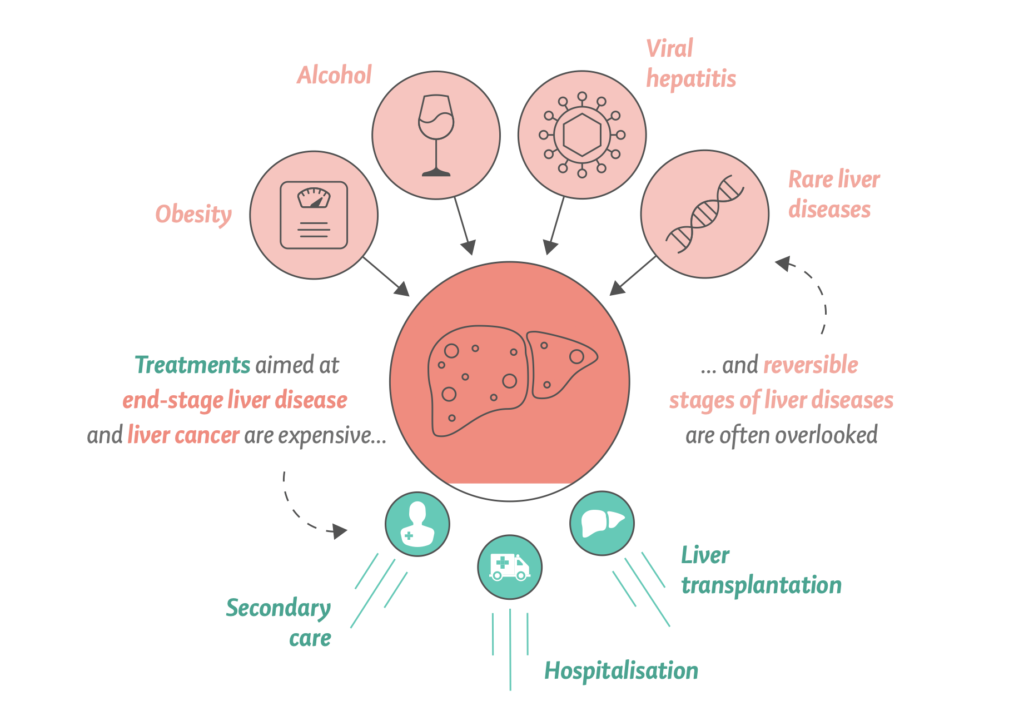
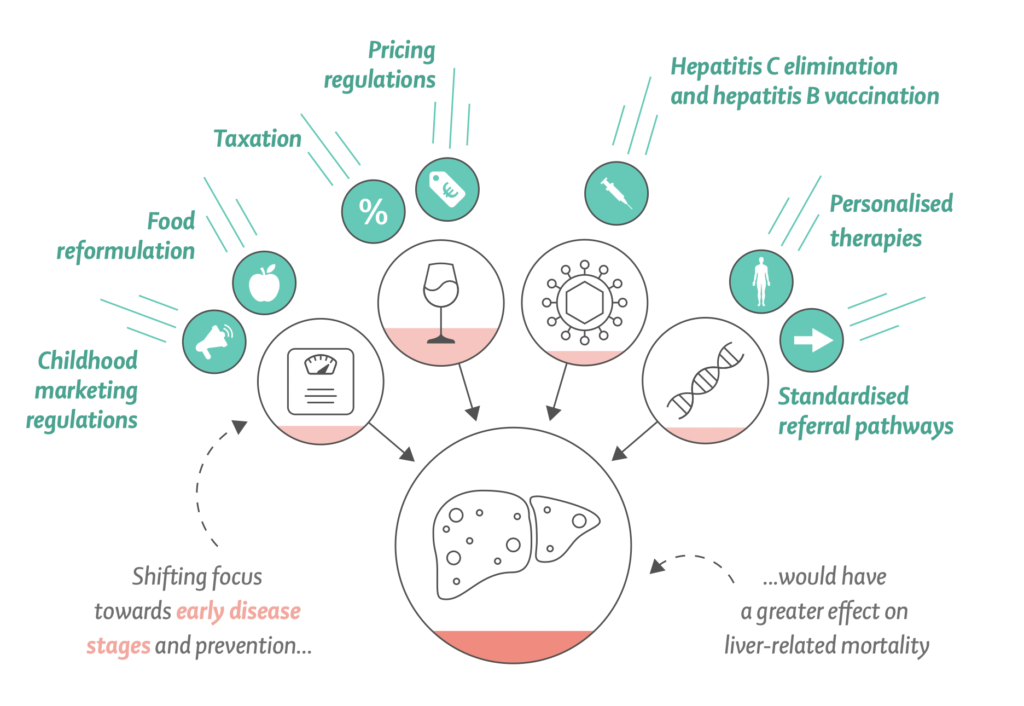
The Liver Commission says targeting end-stage liver disease with high-cost interventions is less effective at reducing liver-related mortality. Instead, the Liver Commission recommends a strategy focused on tackling the main causes of liver disease. Such an approach was cheaper to implement, and had a substantially greater effect.
Liver health is a window to the general health challenges of Europe in the 21st century. We are at the precipice of failure or opportunity. Common risk factors for liver disease reflect behaviours and conditions that are the consequence of both unhealthy environments and social inequities that straddle a wide range of associated medical conditions such as diabetes and cancer.”
Prof. Thomas Berg, Secretary-General, European Association for the Study of the Liver (EASL) and Head of the Department of Hepatology, University Hospital in Leipzig, Germany
Mortality from alcohol-related liver disease is substantially greater for disadvantaged socioeconomic groups, particularly for younger patients, resulting in major health inequalities.
The COVID-19 pandemic has also brought with it physical restrictions that might create environments that lead to increased alcohol consumption. Recently, a U.S. study provided evidence for an alarming increase in Alcoholic Hepatitis associated with increasing heavy alcohol use during COVID-19 and highlighted the need for public health interventions around heavy alcohol consumption.
Such change in liver disease and deaths are entirely consistent with increases in alcohol consumption predominantly impacting on those with the highest alcohol intake. The case for action for liver disease is even stronger as a result.
Paradigm shift towards prevention
The medical profession needs to change its approach to liver disease: instead of focusing on the management of end-stage complications, it needs to shift towards prevention, proactive case-finding, with early identification of progressive liver fibrosis, early diagnosis and early treatment. Therapeutic nihilism for liver diseases belongs to the past.
President of the European Commission, Ursula von der Leyen, emphasized the importance of prevention of chronic diseases in general and liver disease in particular, to promote health and well-being for all Europeans and greater quality of life.
Each year, almost 300,000 people in Europe die prematurely due to problems of the liver. Many of them could have lived longer and healthier lives. Because today, in most European countries, there is good access to secondary care. And in most cases, liver disease can be prevented. Prevention is the best cure that we have. So together, we need to raise more awareness of the preventable and treatable nature of many chronic illnesses.”
Ursula von der Leyen, President, European Commission
Far beyond the liver, alcohol and ultra-processed foods represent key health challenges in the 21st century, and it is increasingly clear that liver disease acts as a cipher for health and a sentinel for our public health capacity.
Europe has the highest rates of alcohol consumption per person the highest prevalence of heavy episodic alcohol use, and the lowest rates of abstention from alcohol in the world. Alcohol combines synergistically with obesity and other risk factors for liver disease to drive the current high rates of end-stage liver disease and liver cancer. Alcohol causes about 40% of the 287,000 premature liver-related deaths in Europe every year, although the true number might be higher.
The OECD model projects:
- Healthy life expectancy to be ca. 1.3 years lower over the next 30 years because of deaths due to liver diseases, with 46% of the reduction as a result of alcohol consumption and 28% as a result of obesity.
- On average, 10.5 million life years and 8.8 million healthy life years will be lost every year in the EU27 + 5 because of liver disease.
- The average annual health expenditure for liver disease in the EU27 + 5 countries is €4.3 billion.
- The impact of liver disease on the economy of the same group of countries leads to the loss of the equivalent of 5 million full-time workers per year.
Alcohol policy solutions to prevent and reduce the liver disease burden in Europe
The Liver Commission argues that the liver is a window to the 21st-century health of the European population. Through the proposed syndemic approach to liver disease and social and health inequities in Europe, the liver will serve as a sentinel for improving the overall health of European populations.
The Liver Commission outlines how Europe can move forward with implementation of effective policy action on taxation, food reformulation, and product labelling, advertising, and availability, similar to that implemented for tobacco, to reduce consumption of alcohol, ultra-processed foods, and foods with added sugar, especially among young people.
COVID-19 has shown the need for public health action and the direct links that exist between population-level interventions, inequities, and mortality. Arguments often made to oppose such interventions have been refuted by the constant publishing of data showing their effectiveness in real time.
With regards to alcohol, the evidence for equitable public health policies is remarkably consistent, summarised by WHO as best buys:
- Tax increases on alcohol-containing beverages,
- Comprehensive restrictions and bans on alcohol marketing, and
- Restrictions on the availability of retailed alcohol.
Alcohol tax increases and minimum unit price for alcohol have implementation costs that are lower than the corresponding benefits in reduced health expenditure and increased labour force productivity. Alcohol taxes also generate revenues.
Writing in a linked Comment published in The Lancet, Dr Richard Horton, Editor-in-Chief and Dr Sabine Kleinert, Executive Editor, added:
To achieve protection and promotion of liver health more broadly, wide-reaching public health policies, such as labelling of unhealthy food and minimum alcohol unit pricing, need to be implemented against commercial interests and political inertia or entanglement.”
Dr Richard Horton, Editor-in-Chief and Dr Sabine Kleinert, Executive Editor, The Lancet
Prof. Nick Sheron, a member of the Commission and Clinical Advisor to Public Health England, emphasized the importance of alcohol policy solutions in the paradigm shift towards prevention of chronic diseases in Europe.
The European Court of Justice and the UK Supreme Court have found that the most effective means to reduce alcohol harm is to set a minimum unit price per centilitre of alcohol.
Prof. Nick Sheron, member of the Liver Commission and Clinical Advisor to Public Health England
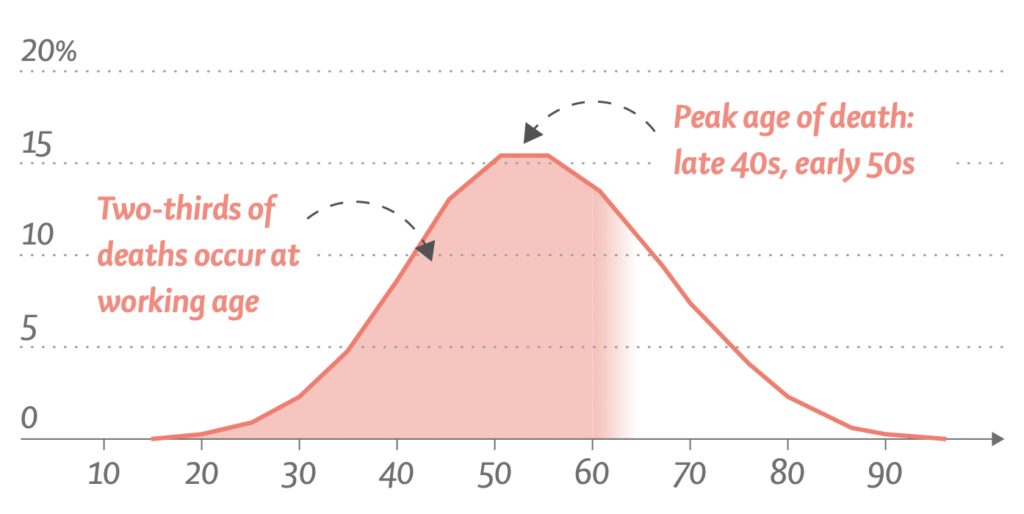
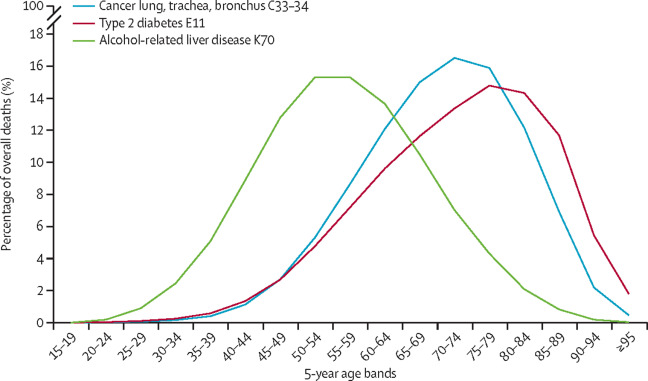
In Europe, chronic liver disease has a substantial impact on young and middle-aged individuals in their prime working years, with the peak age of death occurring in the late 40s and early 50s. This contrasts with mortality from smoking-related and other obesity-related illnesses, such as lung cancer or type 2 diabetes, for which deaths typically occur in the 60s and 70s.
Consequently, data from the World Health Organization shows that liver disease is now second only to ischemic heart disease as the leading cause of years of working life lost in Europe. On average, two-thirds of all potential years of life lost due to mortality from liver diseases are years of working life.
A long-term vision for liver health is a long-term vision for the health of future generations of all Europeans. To be successful a considerable focus must be put on underserved and marginalised communities, including our children.”
Prof. Phil Newsome, Professor of Experimental Hepatology, University of Birmingham, UK and senior author of the Liver Commission’s report
Ten recommendations for a paradigm shift
On the basis of the data collated in its report, the EASL-Lancet Liver Commission makes 10 key recommendations, approximately half of which are targeted to health professionals, and half of which are oriented to policy-makers.
… a combined European effort supported by European medical societies, the WHO Regional Office for Europe, and the European Commission can reverse the alarming trajectories of risk factors for liver diseases. The ultimate long-term goal must be to prevent liver diseases and protect liver health.”
Dr Richard Horton, Editor-in-Chief and Dr Sabine Kleinert, Executive Editor, The Lancet
- Implementation of standardised and simplified liver blood tests for earlier detection and prompt care.
- Utilization of opportunities created by the hepatitis B and C drugs as well as hepatitis B and A vaccines to achieve viral hepatitis elimination in Europe.
- Increase awareness and provide financial incentives for primary care peers and professionals.
- Non-viral liver diseases must be classified along with other non-communicable diseases (NCDs) to engage appropriate care models.
- All forms and sources of stigma towards people at risk of or with liver disease must be opposed – relevant changes to the medical nomenclature should come first.
- Public disclosure of prices for antiviral drugs throughout Europe would reinforce the WHO / World Health Assembly resolution to improve fairness of market prices.
- European governments must introduce uniform policies to reduce harm due to alcohol.
- A complete social and digital media ban on the marketing of alcohol and ultra-processed, high-fat and high-sugar foods targeted to children.
- Promote industry-led food reformulation and minimisation of social inequities by subsidising healthy foods.
- EU and European governments should prioritise the harmonisation of critical forms of public health interventions and health-related policies across Europe.
More details on how the Liver Commission addresses alcohol harm and policy solutions
- In Europe, alcohol consumption is by far the leading cause of liver-related mortality.
- Europe has the highest levels of alcohol consumption per person, the highest prevalence of heavy episodic alcohol use, and the lowest rates of abstention from alcohol in the world.
- Alcohol was responsible for around 580,000 deaths in 2019 (6.2% of all deaths) in the WHO European region, according to the Global Burden of Disease study modelling.
- Alcohol causes about 40% of the 287,000 premature liver-related deaths in Europe every year,
- but the true number is probably higher.
- Alcohol-related liver disease is the most frequent type of liver disease, being responsible for at least 50% of cirrhosis cases, and is the most common indication for liver transplantation in Europe.
- Nevertheless, research on alcohol-related liver disease is underrepresented, amounting to just 5% of all publications in the area of liver disease (2010–14 assessment).
- At the large European and American liver congresses, alcohol-related liver disease represented only 7% and 4%, respectively, of the research presented.
- Alcohol-related harm correlates with the volume and pattern of alcohol use, with epidemiological studies showing an exponential dose–response relationship between alcohol and liver disease.
- For most countries in the WHO European region, there is a strong correlation between liver-related mortality rates and population-level alcohol consumption.
- The evidence linking liver-related mortality and population-level alcohol consumption sends a crucial message for disease prevention:
- alcohol-related cirrhosis is a dose-related condition at the population level, and the most effectual and cost-effective means to reduce mortality rates from alcohol-related liver disease are interventions that reduce population-level alcohol consumption.
Source Website: European Association for the Study of the Liver (EASL)