Changes in the alcohol-specific disease burden during the COVID-19 pandemic in Germany: interrupted time series analyses
Journal article
Summary and meaning
This study answers the question:
What was the impact of the COVID-19 pandemic on hospitalizations and deaths due to alcohol in Germany?
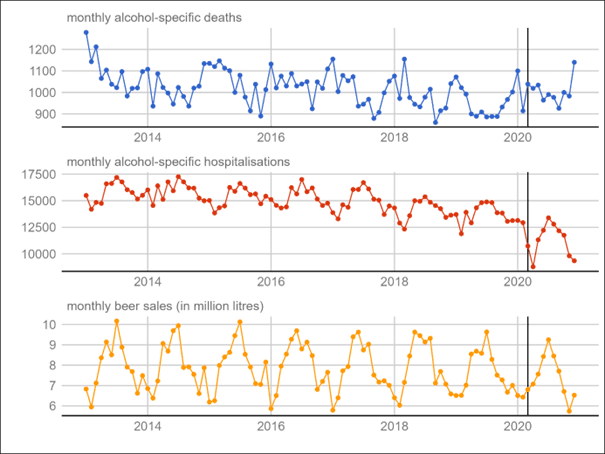
The study analyzed monthly data on – acute (mostly acute intoxication/ poisoning) and – chronic (mostly alcoholic liver diseases and alcohol use disorder) conditions that are specific to alcohol. The researchers did not consider injuries and other health outcomes due alcohol for this study.
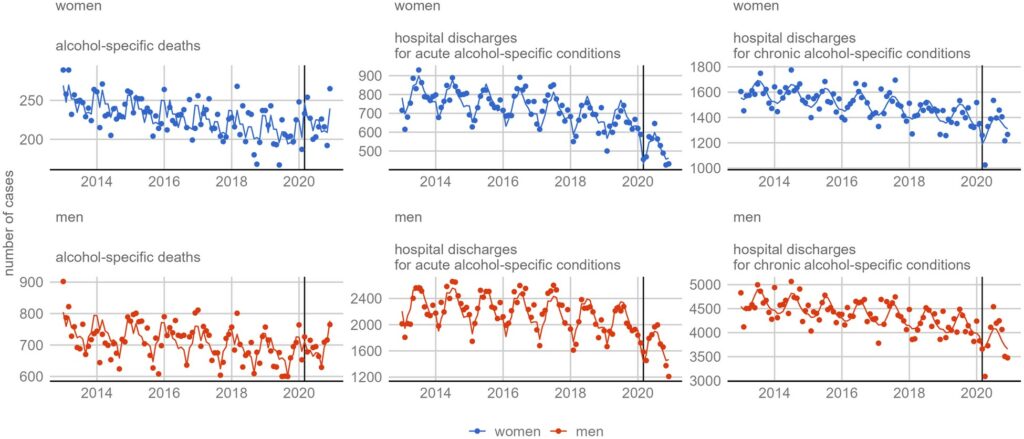
Using interrupted time series analyses, the study shows that hospital discharges for alcohol-specific conditions have plummeted after March 2020. This was more pronounced for acute (-23%) than for chronic conditions (-8%). The study finds this for both sexes in age groups 15-44 and 45-74.
While hospital discharges decreased, the study shows that the death toll for women ages 45-74 increased.
- Deaths due to alcohol in women ages 45-74 have increased by 11%.
- Among younger adults and in both sexes, deaths from alcohol-specific conditions increased by 20-34%.
A lower number of hospitalisations for acute alcohol conditions may reflect changes in alcohol consumption patterns, driven by a reduced number of social events on which people consume (high-risk amounts and patterns) alcohol, e.g., in bars, or on festivals.
A lower number of hospitalisations for chronic alcohol conditions, however, may be indicative of an undertreatment of people with alcohol use disorders during the beginning of the pandemic. Lack of adequate health care may have contributed to rising death tolls.
But with the chosen approach of the study, researchers cannot test their hypothesis that under-treatment was linked to increased alcohol mortality. In fact, there are other factors at play, such as increased alcohol use by vulnerable populations.
Key points
- In Germany, alcohol-specific mortality increased while alcohol-specific hospitalizations decreased with the onset of the coronavirus disease 2019 pandemic in 2020.
- Changes in alcohol use among people with chronic heavy alcohol use patterns in conjunction with an underutilization of addiction-specific services are possible explanations.
- In times of public health crises, access to specialized healthcare services for vulnerable populations such as people with alcohol use disorders should be maintained.
Abstract
Background
The coronavirus disease 2019 pandemic has been linked to changes in alcohol consumption, access to healthcare services and harm due to alcohol.
In this study, researchers quantify changes in alcohol-specific mortality and hospitalizations at the onset of the COVID-19 pandemic in March 2020 in Germany.
Methods
The researchers obtained monthly counts of deaths and hospital discharges between January 2013 and December 2020 (n = 96 months).
Alcohol-specific (International Classification of Diseases, tenth revision codes: F10.X; G31.2, G62.1, G72.1, I42.6, K29.2, K70.X, K85.2, K86.0, Q86.0, T51.X) diagnoses were further split into codes reflective of acute vs. chronic harm from alcohol consumption.
To quantify the change in alcohol-specific deaths and hospital discharges, the researchers performed sex-stratified interrupted time series analyses using generalized additive mixed models for the population aged 45–74. Immediate (step) and cumulative (slope) changes were considered.
Results
Following March 2020, the researchers observed immediate increases in alcohol-specific mortality among women but not among men.
Between the years of 2019 and 2020, the researchers estimate that alcohol-specific mortality among women has increased by 10.8%.
Hospital discharges were analyzed separately for acute and chronic conditions. The total number of hospital discharges fell by 21.4% and 25.1% for acute alcohol-specific conditions for women and men, respectively. The total number of hospital discharges for chronic alcohol-specific conditions fell by 7.4% and 8.1% for women and men, respectively.
Conclusions
Increased consumption among people with heavy alcohol consumption patterns and reduced utilization of addiction-specific healthcare services during the pandemic might explain excess mortality.
During times of public health crises, access to addiction-specific services needs to be ensured.