Temporal Trends in Substance Use and Cardiovascular Disease–Related Mortality in the United States
Research Article
What findings emerged in previous research?
About 10% of the US population have used alcohol or other drugs at some point. Alcohol, opioids, stimulants, sedatives, and cannabis elevate the risk of cardiovascular diseases (CVD), including coronary artery disease, heart failure, and arrhythmias.
Individuals with cardiovascular condition are at high risk. Even though cardiovascular care is getting better, numbers of substance use and substance use-related patients dying from the disease continue to surge.
There is uncertainty about how different types of drugs impact heart health over time. Moreover, the impact of factors like gender, race, and geographical location on this link remain not understood completely.
What is new?
- Substance use and cardiovascular disease–related mortality in the United States between 1999 and 2019 has been on a continuous rise.
- There is heterogeneity in the trend of substance use and cardiovascular disease–related mortality, with women, non‐Hispanic American Indian or Alaska Native individuals, younger individuals, nonmetropolitan area residents, and users of cannabis and psychostimulants having more pronounced increases in substance use and cardiovascular disease mortality.
What are the clinical implications?
- Identifying the high‐risk groups is crucial for prioritizing preventive measures aiming to reduce substance use and cardiovascular disease–related mortality in these populations.
Highlights
Rise in substance use-related cardiovascular deaths revealed in decades-long study
The study spans two decades. This unveils a troubling trend in cardiovascular-related deaths due to alcohol and other drug use. Between 1999 and 2019, overall cardiovascular disease (CVD) deaths decreased, but substance use-related fatalities rose.
Mortality trends
Heart-related deaths not tied to substance use dropped by 1.5% each year. However, deaths linked to substance use rose by 3.9% annually.
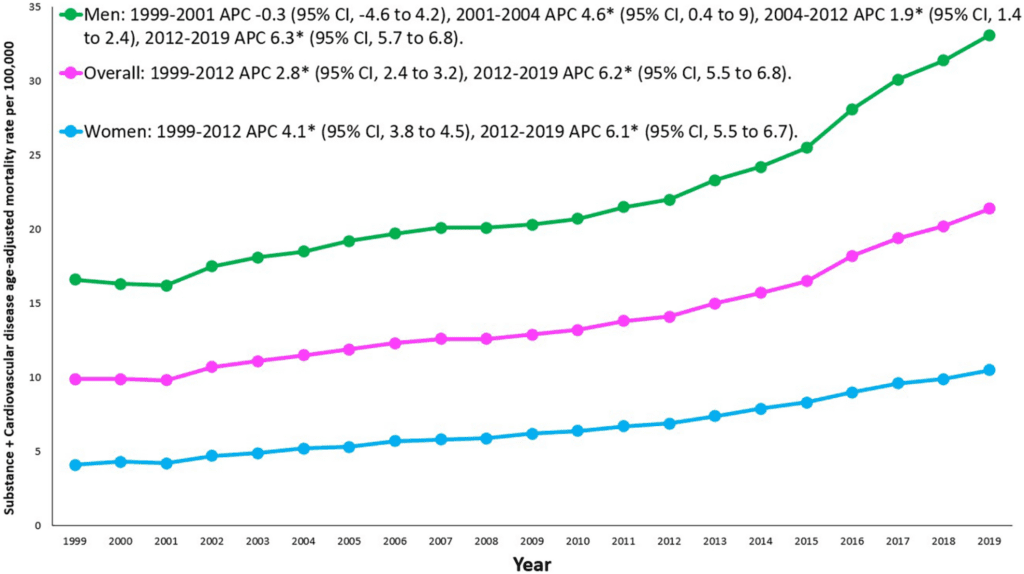
The overall SU+CVD‐related age‐adjusted mortality rates increased from 9.9 in 1999 to 21.4 in 2019 with an average annual percent change of 4.0
The SU and CVD‐related age‐adjusted mortality rate increased from 1999 to 2012 at an annual percentage change of 2.8, which then accelerated to 6.2 from 2012 to 2019. The SU+CVD‐related age‐adjusted mortality rate increased between 1999 and 2019 in both women (annual percentage change 4.8%) and men (annual percentage change 3.6%).
At-risk demographics
Outside the city annual death rate of SU-CVD climbed by 5%, while in the city it rose by 3.8%.
Ethnicity
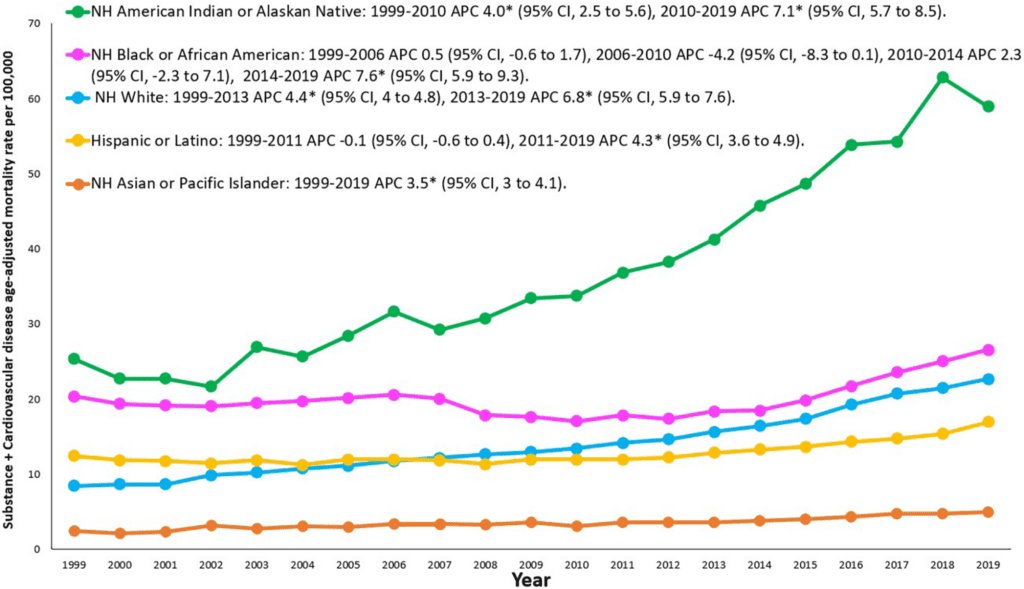
Certain ethnic groups’ death rate has increased. The heart-related death rate due to alcohol and other drugs among American Indian or Alaska Native individuals ranked at the top at 5.4%, followed by NH White individuals at 5.1%.
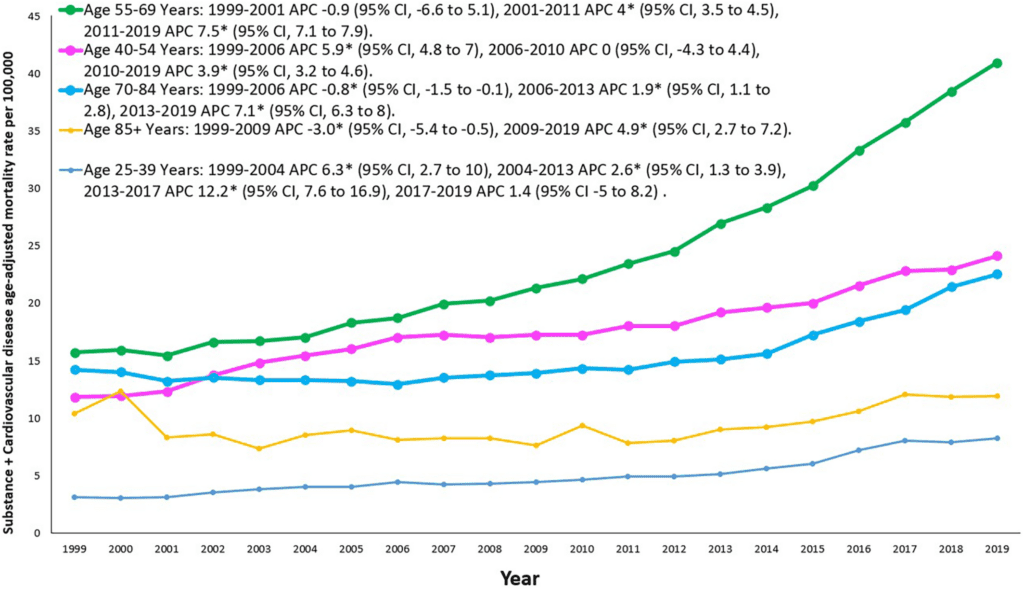
Age
Among SU+CVD deaths, the most common age range was 55 to 69 years (39.1% of SU+CVD‐related deaths), followed by 40 to 54 years (36.8%), 70 to 84 years (12.1%), 25 to 39 years (10.3%), and 85+ years (1.7%).
When stratified by substance category (not mutually exclusive), alcohol accounted for the most SU+CVD‐related deaths (65%), followed by opioids (13.7%), cocaine (9.8%), stimulants (6.5%), sedatives (4.1%), and cannabis (0.5%).
Substance type
Certain substances such as cannabis had the highest increase (12.7%), followed by sedatives (9.4%), opioids (8.7%), cocaine (5.1%), and alcohol with the lowest increase (2.7%).The chart below shows the increase rates by the category of substance.
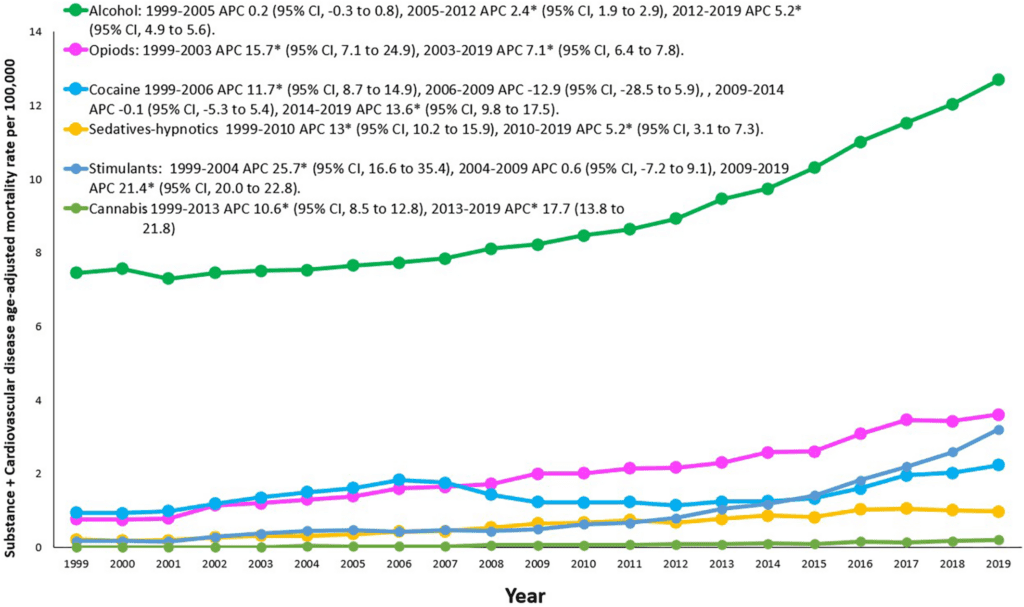
The analysis demonstrates a prominent increase in SU+CVD‐related mortality in the United States between 1999 and 2019, with the most pronounced increases among women, American Indian or Alaska individuals, younger individuals, those living in nonmetropolitan areas, and users of cannabis and psychostimulants.
When looking at the most recent data in year 2019, the age‐adjusted mortality rate (AAMR) was higher among men, American Indian or Alaska Native individuals, those 55 to 69 years old, nonmetropolitan areas, and users of alcohol, opioids, stimulants (methamphetamines), and cocaine.
Additional public health efforts targeting SU may be valuable to reduce CVD mortality.
Abstract
Background
There are limited data on substance use (SU) and cardiovascular disease (CVD)–related mortality trends in the United States. The researchers aimed to evaluate SU+CVD–related deaths in the United States using the Centers for Disease Control and Prevention Wide‐Ranging, Online Data for Epidemiologic Research database.
Methods and Results
The Multiple Cause‐of‐Death Public Use record death certificates were used to identify deaths related to both SU and CVD. Crude, age‐adjusted mortality rates, annual percent change, and average annual percent changes with a 95% CI were analyzed. Between 1999 and 2019, there were 636,572 SU+CVD‐related deaths (75.6% men, 70.6% non‐Hispanic White individuals, 65% related to alcohol).
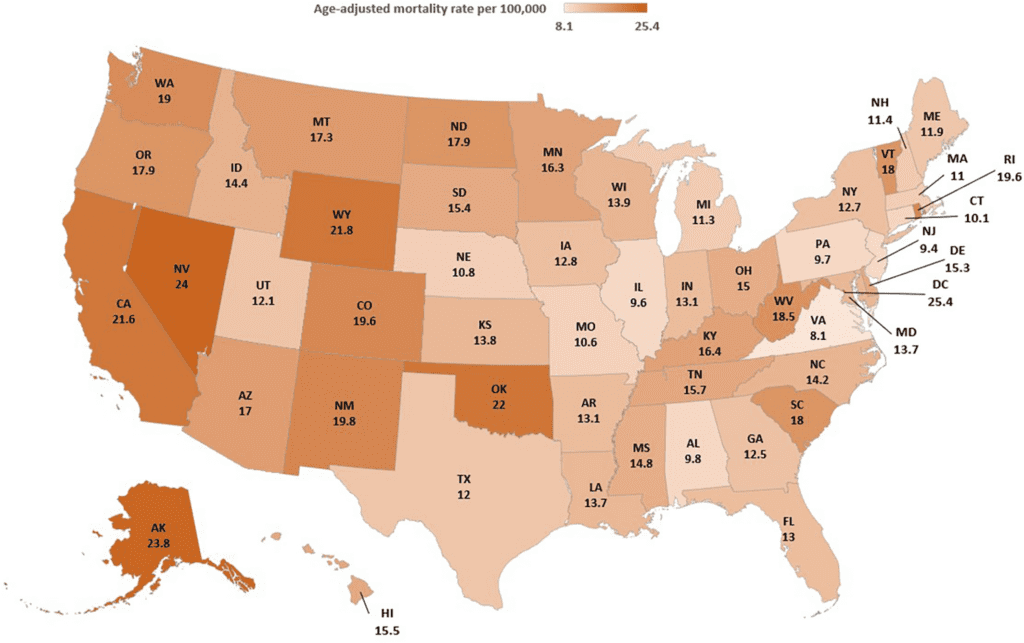
Age‐adjusted mortality rates per 100,000 population were pronounced in men (22.5), American Indian or Alaska Native individuals (37.7), nonmetropolitan/rural areas (15.2), and alcohol‐related death (9.09).
The overall SU+CVD‐related age‐adjusted mortality rates increased from 9.9 in 1999 to 21.4 in 2019 with an average annual percent change of 4.0.
Increases in SU+CVD‐related average annual percent change were noted across all subgroups and were pronounced among women (4.8%), American Indian or Alaska Native individuals, younger individuals, nonmetropolitan areas, and cannabis and psychostimulant users.
Conclusions
There was a prominent increase in SU+CVD‐related mortality in the United States between 1999 and 2019. Women, non‐Hispanic American Indian or Alaska Native individuals, younger individuals, nonmetropolitan area residents, and users of cannabis and psychostimulants had pronounced increases in SU+CVD mortality.
