Syndemic violence victimization, alcohol and drug use, and HIV transmission risk behavior among HIV-negative transgender women in India: A cross-sectional, population-based study
Research article
Summary
In this large, cross-sectional, probability-based analytical sample of HIV-negative transgender women in India, the researchers tested a model of synergistically interacting epidemics, based on the joint effects of four psychosocial exposures – physical and sexual violence victimization, illicit drug use, and alcohol use – on condomless anal sex (CAS). The high prevalence of these adverse psychosocial exposures, their frequent co-occurrence, and their synergistic interactions support the hypothesis that a syndemic is present in this population.
The researchers found evidence of three-way synergistic interactions between physical violence victimization, sexual violence, and alcohol use; and between physical violence victimization, illicit drug use and alcohol use.
The findings suggest that a harmful social-structural environment for transgender women in India contributes to clustering of psychosocial health challenges significantly associated with increased HIV risk, with ramifications for targeted HIV prevention initiatives.
Abstract
Transgender women globally are disproportionately burdened by HIV. Co-occurring epidemics of adverse psychosocial exposures accelerate HIV sexual risk, including among transgender women; however, studies using additive models fail to examine synergies among psychosocial conditions that define a syndemic.
The researchers examined the impact of synergistic interactions among 4 psychosocial exposures on condomless anal sex (CAS) among transgender women in India. A national probability-based sample of 4,607 HIV-negative transgender women completed the Indian Integrated Biological and Behavioural Surveillance survey, 2014−2015.
The researchers used linear probability regression and logistic regression to assess 2-, 3-, and 4-way interactions among 4 psychosocial exposures (physical violence, sexual violence, illicit drug use, and alcohol use) on condomless anal sex (CAS).
Overall, 27.3% reported physical and 22.3% sexual violence victimization (39.2% either physical or sexual violence), one-third (33.9%) reported frequent alcohol use and 11.5% illicit drug use.
Physical violence was associated with twofold higher odds of condomless anal sex (CAS) in the main effects model.
Statistically significant two- and three-way interactions were identified, on both the multiplicative and the additive scales, between physical violence and illicit drug use; physical and sexual violence; physical violence, sexual violence, and alcohol use; and physical violence, alcohol use and illicit drug use.
Physical and sexual violence victimization, and alcohol and illicit drug use are highly prevalent and synergistically interact to increase CAS among HIV-negative transgender women in India.
Targeted and integrated multilevel initiatives to improve the assessment of psychosocial comorbidities, to combat systemic transphobic violence, and to provide tailored, trauma-informed alcohol and substance use treatment services may reduce HIV risk among transgender women.
What the study says about alcohol specifically
In the Indian context, harmful social conditions such as societal stigma faced by transgender women may lead to clustering of psychosocial challenges, such as violence victimization, alcohol use problems, depression, suicidal ideation and attempts, and HIV risk; these may mutually reinforce one another and synergistically amplify the overall disease burden in this population.
Transgender women in India have a high prevalence of psychosocial health challenges, including lifetime physical or sexual violence victimization (84%), alcohol use (37%) and depression (35%), all of which have demonstrated significant additive effects on HIV risk.
Co-occurrence of adverse psychosocial exposures
Among the 4,607 HIV-negative transgender women, irrespective of other exposures, more than one-fourth (27.3%) reported having been exposed to physical violence and 22.3% to sexual violence. More than one-third (39.2%) had been exposed to either physical or sexual violence and 10.5% to both physical and sexual violence.
Over one-third (33.9%) reported frequent alcohol use and 11.5% reported drug use.
Table 3 illustrates the co-occurrence of physical violence, sexual violence, frequent alcohol use, and illicit drug use.
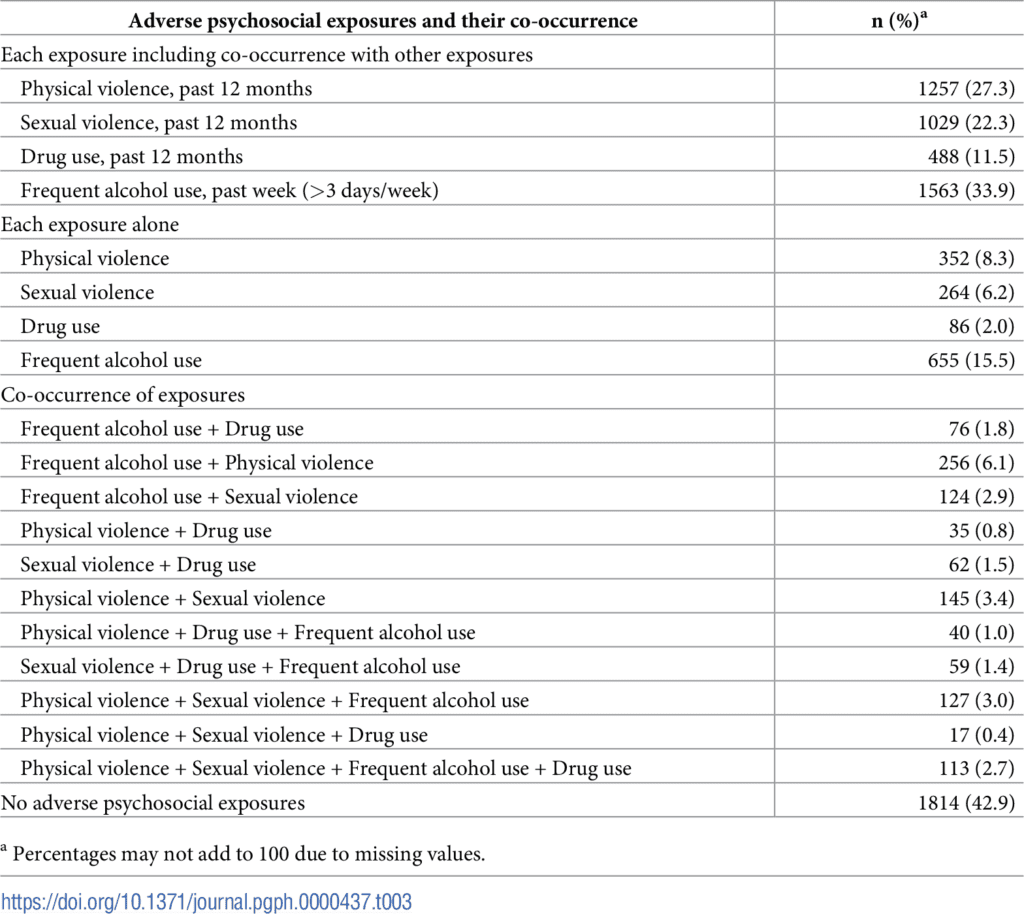
https://doi.org/10.1371/journal.pgph.0000437.t003
The study demonstrates that multiple forms of violence victimization against transgender women, and in conjunction with illicit drug use and alcohol use, contribute to synergistically increasing HIV risk.
The links identified using models of synergistically interacting epidemics have been demonstrated among transgender women in other countries.
- For example, studies among transgender women in North and South America indicate that life stressors, discrimination, and trauma can lead to alcohol and/or substance use, possibly as maladaptive coping strategies.
- Several other studies with transgender women, showed that alcohol use and illicit drug use, were associated with increased HIV risk.
- As identified among other populations, such as gay and bisexual men, being under the influence of alcohol or illicit drugs may increase the likelihood of engaging in sex and the risk of condomless anal sex (CAS).
- Thus, experiences of sexual violence can precipitate alcohol use as a coping mechanism, and alcohol use (especially before or during sex) in turn may increase the likelihood of being targeted or otherwise exacerbate sexual or physical violence from male partners, which increases the risk of engaging in condomless anal sex (CAS).
Implications for practice and policy
Given that larger societal forces, such as systemic stigma and discrimination, economic marginalization, etc., contribute to violence victimization – as well as indirectly leading to alcohol and illicit drug use through internalized stigma and depression – addressing these social and structural factors is crucial.
Currently, ‘crisis response’ teams established in NACO-supported targeted HIV interventions act only after incidents of violence are reported. The researchers are not aware of any societal-level campaigns in India designed to prevent discrimination and violence against transgender women in relation to their intersecting marginalized identities (e.g., gender minority and sex worker and/or HIV-positive status).
The study findings further indicate that physical violence victimization independently, and together with sexual violence, illicit drug use and alcohol use synergistically increase condomless anal sex (CAS). That is, in the presence of physical violence victimization, relatively higher levels of CAS were observed with one or more combinations of sexual violence victimization, illicit drug use and/or alcohol use.
Thus, addressing all four exposures through integrated, multicomponent interventions may substantially reduce HIV risk.
However, in the context of synergistic interactions, single-component interventions (e.g., post-care support for survivors of sexual violence or treatment of alcohol or other drug dependence) may still exert an incremental impact on reducing HIV transmission risk behavior.
Partial support for the model of serially causal epidemics – i.e., sexual violence victimization leading to alcohol and other drug use, and possible mutually causal associations between violence victimization and drug use – suggest the utility of multilevel interventions:
- at the individual level, screening for and managing alcohol and illicit drug use; and
- at the societal level, strengthening stigma and violence reduction or elimination programs.
Although alcohol use and illicit drug use were not independently statistically significant predictors of CAS (main effects model), in the presence of sexual and/or physical violence victimization, alcohol use and/or illicit drug use substantially increased CAS.
Nongovernmental (NGOs) and community-based (CBOs) organizations that implement targeted HIV preventive interventions for transgender women should establish or strengthen referral systems with public hospitals offering treatment for alcohol and illicit drug dependence, post-violence (physical or sexual) support services, and post-sexual exposure prophylaxis (PEP).
To this end, training and monitoring healthcare providers to ensure nondiscriminatory and gender-affirmative care is crucial. Similarly, support is required from police in duly filing complaints of sexual or physical violence, given that transgender persons are not covered in current sexual assault/rape laws (Indian Penal Code, Section 354) – a pernicious lapse in legal policy.
Further, in addition to HIV and condom education and condom distribution, NGOs and CBOs should educate transgender women about the negative effects of alcohol and illicit drug use on sexual decision-making and negotiation, and counsel and support them to reduce or avoid illicit drug or alcohol use before or during sexual encounters.
