The Director of the Pan American Health Organisation (PAHO) Dr. Jarbas Barbosa has emphasised the need for a new agenda for mental health in the Americas. The new agenda recommends alcohol policy action to address worsening mental health in the region.
The mental health of the population of the Americas has been severely impacted by the COVID-19 pandemic, and its effects on our lives, economies and societies.”
Dr. Barbosa, Director for the Pan American Health Organisation
Dr. Barbosa made these statements at a media briefing to launch a report on behalf of PAHO. The report was titled ‘A New Agenda for Mental Health in the Americas’. The report is the culmination of the High-Level Commission on Mental Health and Covid-19. It was established in May 2022 by PAHO.
The Commission consisted of 17 experts from government, civil society, academia and those with lived experience of mental health conditions.
The Commission provided guidance to PAHO and its Member States on how it could advance mental health in the Region during and after the pandemic.
Poor mental health represents a significant source of disability and mortality in the American region.
Unfortunately, the majority do not receive the care they need. It is estimated that more than 80% of people suffering from severe mental health conditions did not receive treatment.
Mental Health and Alcohol: A Heavy Burden
The report states that unmet mental health needs are a significant contributor to the disease burden in the region. Mental, neurological, and substance use conditions, as well as suicide account for more than one-third of total years lived with disability (YLDs) in the region. They also accounts for a fifth of total disability-adjusted life years (DALYs) in the Americas.
Alcohol consumption plays a significant role in these numbers:
- 8.2% of the general population over 15 years of age, for example, suffer from an alcohol use disorder.
- The prevalence rate for alcohol use disorders among women is the highest of all the WHO regions.
- It is also the second highest among men.
- It is estimated that 5.5% of all deaths and 6.7% of DALYs are attributable to alcohol consumption.
The Gender Dimension of Mental Health and Alcohol
A person’s gender has implications for mental health across the course of every person’s life. However, gender inequalities affect women and girls are disproportionately. Women in the Americas continue to experience an unfair distribution of opportunities and resources compared to men. Gender norms expose vulnerable individuals to mental health risks. It also negatively affects their help-seeking behaviours, and ultimately, their mental health outcomes.
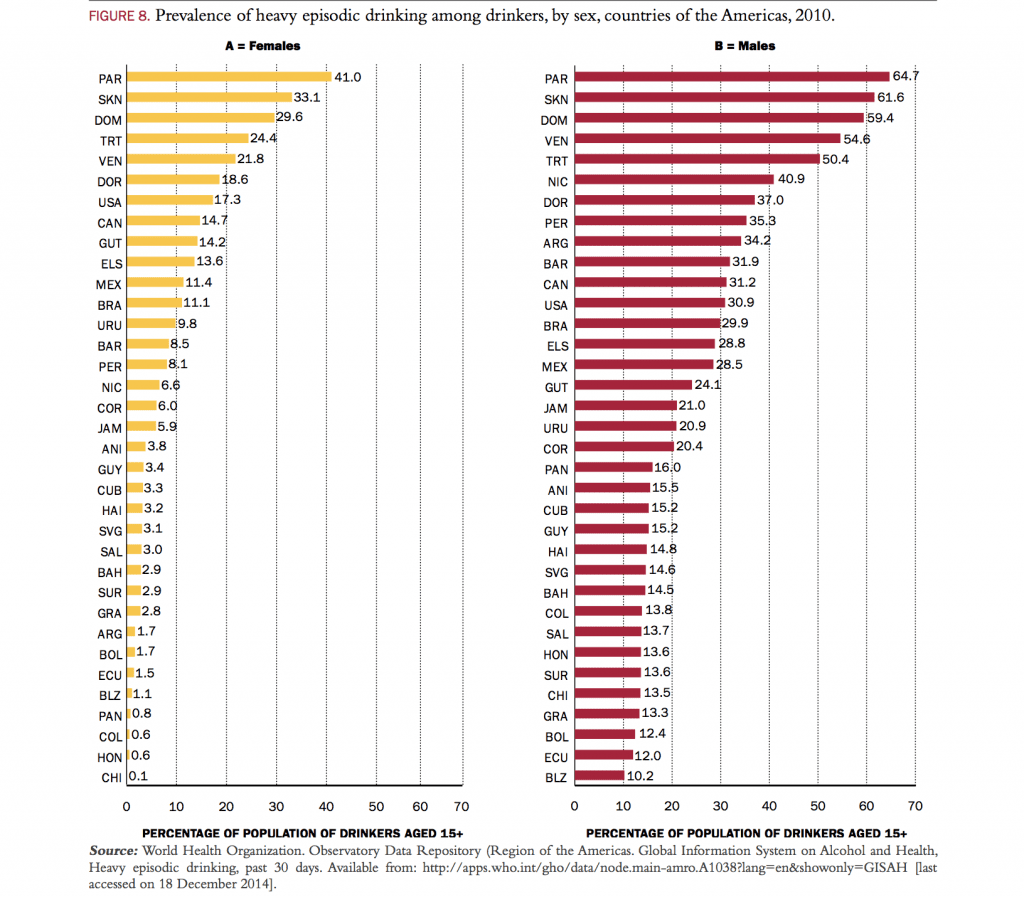
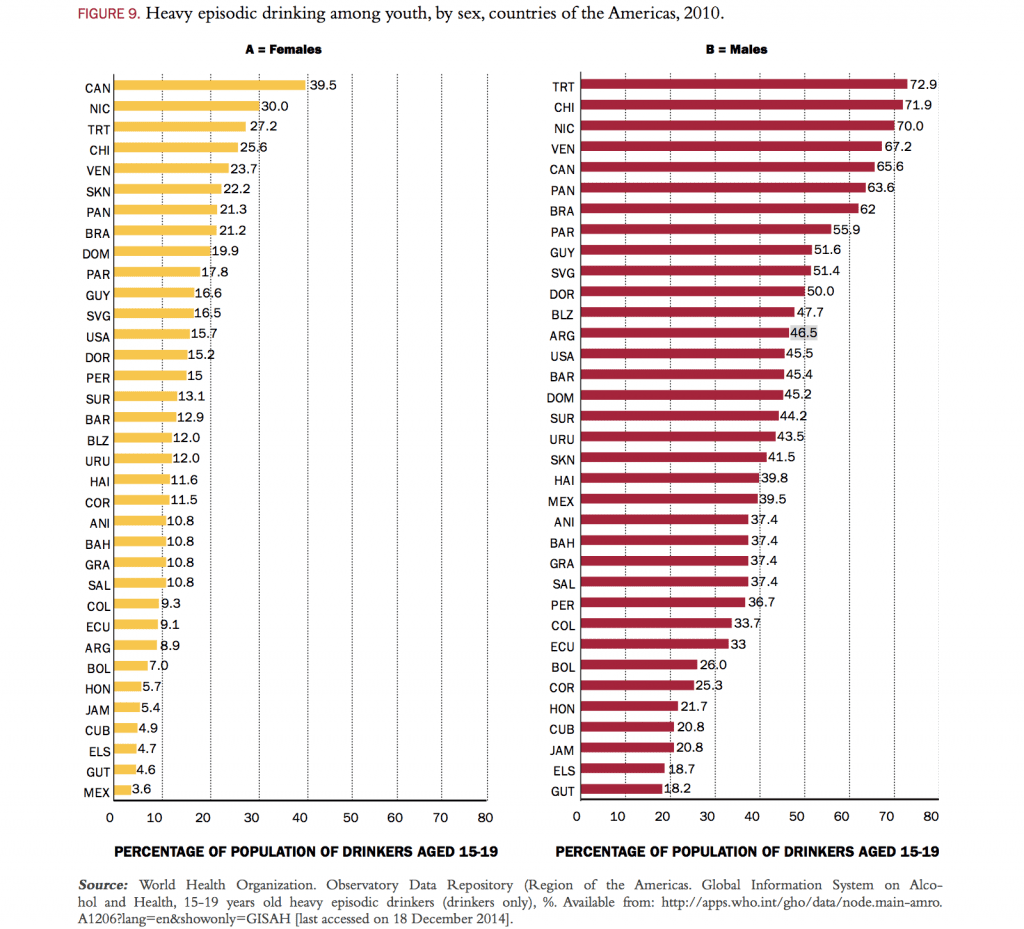
Men, too, experience mental health outcomes influenced by their gender. The prevalence of alcohol use disorder in men in the region for example is more than double than that of women. Men are also more than three times as likely to die by suicide, although women are more likely to make a suicide attempt. Behaviours rooted in socially constructed masculinities also expose men to risks such as suicide, alcohol use and other addictions.
The mental health of diverse gender identities, expressions, and sexual orientations is also an important facet to consider. The LGBTQ+ community is more likely to experience human rights violations and discrimination. They also face denial of care, discriminatory attitudes, and inappropriate pathologizing in healthcare settings. LGBTQ+ persons experience mental health disparities including higher rates of depression, anxiety, alcohol use disorder, suicide, and suicidal ideation. This may be due to factors such as chronic stress, social isolation, and a lack of connection with various health and support services.
Financing the New Agenda for Mental Health in the Americas
Currently, funding for mental health in the Americas falls short of meeting the need for it. This is demonstrated by the high burden of mental health conditions and the large number of affected people and the people that receive care.
The average ratio of the mental health burden to expenditure on mental health is 6:1. This means that the burden attributable to mental health conditions is six times the proportion of health funds allocated to mental health.
The report puts forward suggestions on how financing for mental health can be increased. These include leveraging existing funding sources as well as establishing new ones.
One such avenue for finance suggested is through sales or excise taxes on harmful products.
The report describes how increased taxation on tobacco, alcohol, and sugary drinks would have the added benefit of reducing the consumption of products that contribute to disease and premature mortality.
Strengthening Public Policy to Reduce Key Risk Factors for Suicide
Governments have the ability to address some of the key risk factors for suicide, especially direct access or proximity to means for suicide. According to the report, limiting access to the means of suicide is a universal evidence-based intervention for preventing suicide.
Alcohol use is an important risk factor for suicide that can be protected against through high-impact, proven public policy.
- The risk of a suicide attempt is estimated to be around seven times greater soon after consuming alcohol.
- It increases to 37 times after heavy use of alcohol.
In 2018, WHO, in collaboration with international partners including Movendi International, launched the SAFER Initiative, to provide support for countries in preventing and reducing alcohol harm. The initiative seeks to strengthen the ongoing implementation of the WHO Global Alcohol Strategy and other WHO and United Nations instruments.
Alcohol, Mental Health Conditions, and Policy Solutions
There are associations of alcohol use and alcohol use disorders (AUD) with almost every mental disorder, including depression, post-traumatic stress disorder (PTSD) and suicide.
According to the WHO Global Alcohol Status report from 2018, alcohol use disorder is pervasive.
In 2016, an estimated 283 million people aged 15+ years had an AUD. That equals 5.1% of all adults worldwide.
The past 12-months prevalence of AUDs was the highest in the WHO European Region and in the Region of the Americas.
- Europe: 66.2 million people aged 15+ years, representing 8.8% of the population of that age group.
- Americas: 63.3 million, representing 8.2% of the population aged 15 years and older
Alcohol dependence – the most severe form of AUD – occurred in 2.6% of people of aged 15+ years in 2016.
- Americas: 4.1% prevalence of alcohol dependence, and
- Europe: 3.7% prevalence of alcohol dependence.
In many countries of the Americas region, such as the United States, communities are facing the formation of a perfect storm of factors driving alcohol use disorders to higher rates than ever seen before – the so called “triple trouble” of a pandemic, unemployment, and diminished personal and community support services for people affected by substance use problems.
Mental health experts are anticipating a steep rise in alcohol harm, suicides, domestic violence and depression that could rival the toll from COVID-19 itself. All this is by political design, as law makers favor Big Alcohol’s profits over communities’ health services.
In the U.S., for instance, the COVID-19 pandemic has caused alcohol and other substance use to rise. As a result, the demand for alcohol use disorder support services has steadily increased during the pandemic. But services have not been able to keep up with rising demand.
A 2022 survey found that 43% of U.S. adults who say they needed substance use or mental health care in the past 12 months did not receive that care. Urgent action is needed to ensure people and communities who require substance use and mental health care receive the support they need.
A growing body of research points to the direct link between alcohol and suicide.
Policy action to limit the availability of alcohol and to reduce the affordability of alcohol is a solution to reduce the number of suicides, studies show.
Already in 2016 evidence from a review of existing study literature indicated that alcohol policy measures ought to be discussed when searching for suicide prevention measures. The study was published in the journal Alcoholism: Clinical and Experimental Research.
There’s ample literature [on alcohol and suicide]. What’s missing is how alcohol policy affects suicide,” said study author Ziming Xuan, an assistant professor of community health sciences at Boston University’s School of Public Health.
Ziming Xuan, assistant professor of community health sciences, Boston University’s School of Public Health
If the total consumption level of a population can be reduced, the suicide risk can be shifted in a population level. Availability and affordability of alcohol matter. The more difficult it is to obtain alcohol, and to afford alcohol, the less people will purchase and consume and consequentially the fewer alcohol-related suicides will occur.
In his analysis, “Alcohol Policies and Suicide: A Review of the Literature”, Xuan reviewed 17 studies on alcohol policies and suicide published between 1999 and 2014.
The analysis showed that policies like alcohol taxation, limiting the number of stores that sell alcohol in a given area, increasing minimum ages for alcohol use, and limiting hours for alcohol sales were associated with lower suicide rates.
The SAFER Technical Package
The SAFER technical package identifies five key alcohol policy interventions based on accumulated evidence of their impact on population health and cost-effectiveness.
- Strengthening restrictions on alcohol availability,
- Advance and enforce alcohol-impaired driving countermeasures,
- Facilitate access to screening, brief interventions, and treatment,
- Enforce bans or comprehensive restrictions on alcohol advertising, sponsorship, and promotion, and
- Raise prices on alcohol through excise taxes and other pricing policies.
From an alcohol policy perspective, it is significant to note the role that alcohol plays in exacerbating crisis such as mental health issues. However, addressing alcohol through proven policy solutions has the potential to alleviate these same issues and to promote health and well-being for all.
Sources
Pan American Health Organisation Official Website – Mental Health Must Be Top of The Political Agenda Post-COVID-19, PAHO Report Says
A New Agenda for Mental Health in the Americas: Report of the Pan American Health Organization High-Level Commission on Mental Health and COVID-19 (Official Publication, PDF)