Massive alcohol-related cancer mortality
There are almost 240,000 cancer deaths due to alcohol every year in the nine countries with the biggest burden. These nine countries combine for a population of almost 3 billion people, nearly half the global population.
The death rate from alcohol-related cancers is astonishingly high. According to WHO’s 2018 Global Alcohol Status Report, this is the alcohol-related cancer mortality in the nine countries with the biggest burden:
- China: 78.052 cancer deaths due to alcohol (population of 1.4 billion),
- India: 30.958 (population of 1.3 billion),
- USA: 30.859 (population of 327 million),
- Russia: 28.702 (population of 144 million),
- Japan: 20.124 (population of 126 million),
- Germany: 14.696 (population of 82 million),
- Brazil: 13.332 (population of 209 million),
- France: 10.982 (population of 67 million),
- UK: 10.412 (population of 66 million).
These numbers are astonishing and shocking for every single country on the list. In my own country, Germany, 14.000 people die from alcohol-related cancer every year.
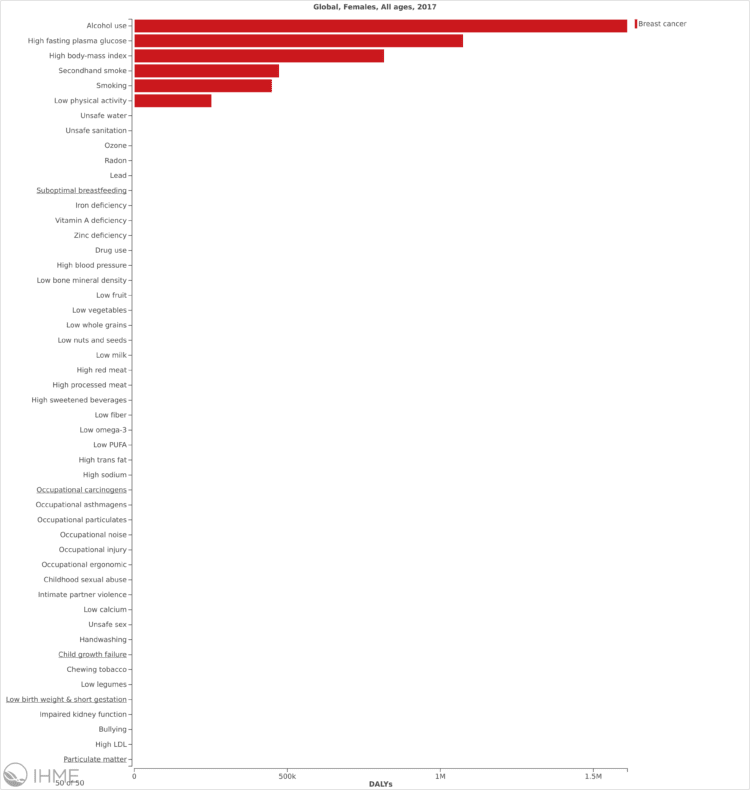
For women globally, alcohol is actually the single biggest risk factor for breast cancer – both in terms of health burden and mortality.*
But there is no public discourse, in fact there is very little public awareness, about this death toll and about the fact that alcohol causes cancer. The scientific community and the World Health Organization know that alcohol is a group one carcinogen – just as asbestos and tobacco smoking – since 1988. But awareness of the link between alcohol and cancer are nowhere near the understanding that the public has about the link between smoking and cancer.
The alcohol-cancer link: a social justice issue
This is a social justice issue as much as it is a public health issue.
Social justice is the concept that relations between an individual and the society they live in should be fair and just – for example in the ways that wealth, opportunities for personal fulfilment, and social privileges are distributed. I think there are three dimensions that show why and how the alcohol-cancer link is a social justice issue.
1. People have a right to know the truth about alcohol
In general, researchers have found that the clarity and accuracy of public health messaging on alcohol lags behind that for tobacco and other drugs. The historical lack of clarity in public health messaging about alcohol consumption is further exemplified by a study recently published in The Lancet, which debunks the widely held misconception that “moderate” alcohol consumption confers beneficial health effects.
Cognitive dissonance about alcohol is a real problem, both on individual and societal level. We hold conflicting attitudes and beliefs about alcohol that affect our behaviors. Alcohol harm is so pervasive that people know concrete examples and likely have experienced it themselves or in their families, workplaces, or leisure time communities. At the same time alcohol is also omnipresent in promotions, glamorizations, and even in cultural myths about its effects. These myths lead to behavior that is often inconsistent with the reality of alcohol’s risk and real harm.
The beliefs about alcohol’s positive effects crowd out awareness of and understanding for alcohol’s real effects, such as cancer.
Understanding of alcohol’s real effects matters for how communities and societies view and recognize alcohol harm and treat alcohol policy solutions.
Maik Dünnbier
For example, in the United States more people attribute stress and other unproven factors leading to cancer than recognize that alcohol has clear links to cancer risk, according to a survey from the American Institute for Cancer Research.
Only 39% of Americans are aware of alcohol’s cancer risk. The low awareness of the alcohol-cancer link is especially concerning given that it has dipped over the past 16 years, from 42% in 2001 to 39% today.
In England, a 2015 survey showed that only 13% of respondents identified cancer as a potential health outcome of alcohol consumption.
But people have the right to know, and not just alcohol consumers. Everyone has a right to know: For example, children and their parents and cancer patients and their doctors and nurses.
Understanding of alcohol’s real effects matters for how communities and societies view and recognize alcohol harm and treat alcohol policy solutions.
The acceptance of potential risk from contaminated water is much lower than the risk people are taking in terms of alcohol consumption. We don’t want to consume tab water that is not entirely safe. But in beer, wine, and liquor, so far, people have no problem consuming a carcinogen like asbestos. It’s because they don’t know and it’s because societies still glamorize ethanol and promote its use everywhere.
Understanding of alcohol’s real effects matters for how parents talk with their children about using and not using, about whether or not to begin alcohol consumption. It matters for how doctors talk with their (cancer) patients and which advice they provide (or do not provide) for cancer survivors to stay healthy. It matters for women, for instance, who have a higher genetical risk of developing breast cancer. And it matters for alcohol consumers, in how much and how often they actually would consume alcohol.
Understanding the risks linked with alcohol consumption is like a vaccin that helps immunize against the negative consequences of this (still) glamorized and heavily promoted vector of disease, disability and death.
Maik Dünnbier
Understanding of the alcohol-cancer link matters for vulnerable people and communities especially. They are more exposed to alcohol harm, have less resources to deal with and overcome harm from alcohol and benefit more from reducing alcohol use, quitting or not even starting alcohol use.
Understanding the real effects of alcohol matters for the norms a society develops for what a healthy and sustainable community is – and what it is not.
Alcohol causes cancer. And there is no safe amount of alcohol use. And there is no amount of alcohol use that is healthy. This fact and understanding matters for anyone who wants to make conscious decisions about a healthy and sustainable way of life, who wants their children to live in healthy environments, who wants to reduce cancer risk due to family history of breast cancer or who is a cancer survivor and needs to prevent reoccurrence.
Understanding the risks linked with alcohol consumption is like a vaccin that helps immunize against the negative consequences of this (still) glamorized and heavily promoted vector of disease, disability and death.
And this protection is essential for people to live healthy, fulfilled, self-determined lives.
2. The alcohol industry does not want people to know their products are carcinogenic
During the spring of 2018 in the region of Yukon, Canada, an alcohol industry pressure campaign led to the termination of a scientific study into the effectiveness of cancer warning labels on alcohol containers. The research was intended to examine how warning labels could influence consumers’ attitudes and behaviours. For eight months, new, more prominent stickers would be attached to cans and bottles of alcohol warning of cancer risks associated with alcohol consumption. The study was supposed to be a public health experiment, backed by Health Canada and Yukon’s chief medical officer of health. The research was part of a larger public health strategy, and Yukon provided an enthusiastic testing ground.
In the aggressive lobby campaign, Beer Canada lied about the alcohol-cancer link, claiming it was a “misleading statement” on the label to say that alcohol can cause cancer. But in an interview, Tim Stockwell, the co-principal investigator of the study and the director of the Canadian Institute for Substance Use Research, reacted to Beer Canada’s claim:
It’s utterly false.
[The American Society of Clinical Oncology] put out a statement in The Lancet recently celebrating 30 years and saying, ‘Why has there been no action? Why is it hardly anybody knows alcohol causes cancer?
This is the reason. Because when you try and put the message out there, it’s squashed.”
Tim Stockwell, co-principal investigator of the study and director, Canadian Institute for Substance Use Research
This is just one example illustrating that the alcohol industry really does not want the broader public to clearly understand the link between alcohol and cancer.
In 2017, a ground-breaking study presented evidence illustrating that the alcohol industry is misleading the public over their products’ cancer risks. The study showed that Big Alcohol and their front groups are working to misrepresent scientific evidence about alcohol-related cancer risks. The tactics they use are very similar to those of the tobacco industry.
The researchers wrote:
The alcohol industry appears to be engaged in the extensive misrepresentation of evidence about the alcohol-related risk of cancer. These activities have parallels with those of the tobacco industry. This finding is important because the industry is involved in developing alcohol policy in many countries, and in disseminating health information to the public, including schoolchildren.
Policymakers, academics, public health and other practitioners should reconsider the appropriateness of their relationships to these alcohol industry bodies.”
Petticrew, M., Maani Hessari, N., Knai, C. and Weiderpass, E. (2017), How alcohol industry organisations mislead the public about alcohol and cancer. Drug Alcohol Rev.. doi:10.1111/dar.12596
The International Agency for Research in Cancer (IARC), the World Health Organization’s special cancer research body, classifies alcohol as category one carcinogen since 1988, like asbestos and tobacco. The IARC estimates that alcohol is the cause of 8% of all cases of cancer. After tobacco (18%), alcohol is the second biggest cause of cancer.
Nevertheless, awareness of alcohol’s cancer risk is very low among the public. For example in Europe, only 1 in 10 people know about the connection between cancer and alcohol.
Blocking scientific research into and systematically misleading about the alcohol-cancer link is still not all Big Alcohol does to keep people from understanding alcohol’s cancer risk. They are also engaging in pink-washing.
Pink-washing is the term for all cases when companies that manufacture and market carcinogenic products engage in “cancer awareness and prevention campaigns”. A study documented alcohol products promoted with pink ribbons, partnerships with breast cancer charities, and general terms such as “breast cancer research” or “cure.” Hundreds of alcohol brands promote products with breast cancer awareness ribbons.
Cynically, pink-washed alcohol brands contribute to cancer risk in the name of research, treatment, and/or prevention. Pink-washed alcohol products extend the potential to increase sales of a carcinogen by linking an iconic charitable cause and entire populations of women, including young women who may already consume alcohol at higher levels.
These industry tactics are exploitative. Big Alcohol has decided to pursue profits by keeping people in the dark about the consequences of their products; to make this worse, they actually work to increase the darkness and sow doubt about scientific knowledge.
This matters from a social justice perspective because open societies rely on informed citizens when they engage in social causes (such as Breast Cancer awareness) and when they engage in policy-making process that affect their communities and societies.
3. Awareness leads to policy support
Alcohol harms extend far beyond cancer. Violence, workplace accidents and injuries, road traffic fatalities, child neglect and abuse, the list is long. But scientific analysis shows that 12.5% of the 3 million annual alcohol deaths are due to cancer.
And research has also indicated that the lack of public awareness of the alcohol-cancer link may contribute to a lack of public support for alcohol policies.
This is what explains the strategy of the alcohol industry to keep people in the dark about their products’ carcinogenicity: fuelling cognitive dissonance and undermining public support for alcohol control measures that would threaten their profits.
In 2018, a study found that support for alcohol policies is greater among individuals who are aware of the link between alcohol and cancer. Scientists concluded:
… a large proportion of people are unaware of the alcohol-cancer link and so increasing awareness may be an effective approach to increasing support for alcohol policies.”
Bates et al. BMC Public Health (2018) 18:688 https://doi.org/10.1186/s12889-018-5581-8
Awareness of the alcohol-cancer link was associated with increased support for alcohol policy measures, such as price and availability regulation and others. The Global Burden of Disease study shows that alcohol causes ca. 650.000 cancer deaths per year, globally.
That clearly means that alcohol policy solutions are real catalysts for cancer prevention.
- For example, reducing total alcohol consumption by 10% would lead to a 9% reduction in alcohol-related cancer deaths. That means ca. 57.000 fewer deaths.**
If this is not a social justice issue, then what is?
Analysis from the United States shows: More restrictive state alcohol policies were associated with lower cancer mortality rates for the six cancer types overall, and among men and women. A 10% increase in the restrictiveness of alcohol policies was associated with an 8.5% decrease in rates of combined alcohol-attributable cancers. Strengthening alcohol control policies may be a promising cancer prevention strategy.
A study from the UK confirmed these effects for breast cancer specifically:
Over 20% of women aged 45 to 64 reportedly consume more alcohol than 14 units per week, so any intervention to reduce population level consumption could have a significant influence on breast cancer rates, as well as help to manage the side effects of treatment and improve the overall health of survivors,” according to the researchers of the study.
When people know about the alcohol-cancer link, their support for alcohol policy measures increases. In turn, these alcohol policy solutions are effective in helping prevent and reduce cancer morbidity and mortality. Moreover, the alcohol policy best buys effect other aspects of alcohol harm, too, reducing the overall alcohol burden on people, families, communities and societies. Even in this dimension, understanding of the cancer risk from alcohol consumption is a social justice issue.
Sources and explanation
* Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization. Seattle, WA: IHME, University of Washington, 2018. Available from http://vizhub.healthdata.org/gbd-compare. (Accessed Feb. 4, 2020)
** We calculated the cancer deaths averted from improved alcohol policy through a 10% and a 30% total per capita alcohol consumption reduction scenario. InterMAHP has a function to test these scenarios.
- Assuming 649,840 alcohol-related cancer deaths in 2017, a 10% reduction of total alcohol use would lead to 9% fewer alcohol-related cancer deaths, meaning 57,300 fewer deaths.
- With a 30% lower total alcohol consumption, calculations show that 26% of alcohol-related cancer deaths could be averted, meaning 171,460 fewer deaths.
